The document provides guidelines for operating theatre practices to prevent surgical site infections. Some key points:
1) Proper infection control practices like preoperative patient shower, nasal decolonization for certain surgeries, appropriate hair removal and antiseptic skin preparation can reduce infection risks.
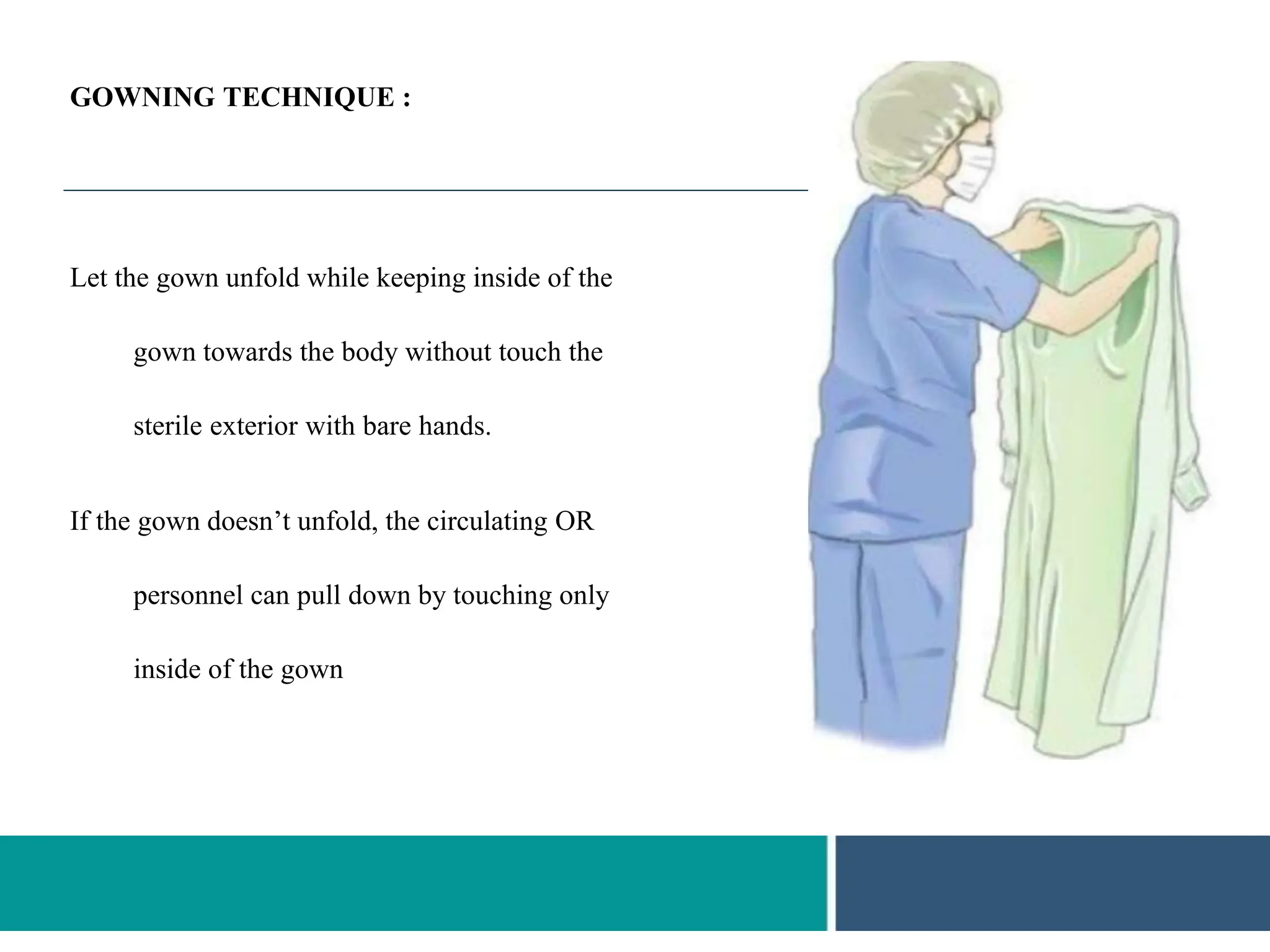
2) Strict adherence to attire, behavioral and environmental standards like proper scrub suits, caps, masks, surgical hand scrubbing and gloving techniques are important for the surgical team.
3) Maintaining optimal temperature, airflow, humidity and air changes in the operating theatre helps control infections. Proper draping and limiting exposure of the surgical site are also recommended.







































































![References
• Over-the-Counter Topical Antiseptic Products: Drug
Safety Communication - FDA Requests Label
Changes and Single-Use Packaging to Decrease Risk
of Infection. US Food and Drug Administration.
http://www.fda.gov/Safety/MedWatch/SafetyInformat
ion/SafetyAlertsforHumanMedicalProducts/ucm37489
2.htm. Accessed February 11, 2015.
• Guideline for a safe environment of care, part 1. In:
Guidelines for Perioperative Practice. Denver, CO:
AORN, Inc; 2015: 239-263. [IVA]
• Gottardi W. The influence of the chemical behaviour
of iodine on the germicidal action of disinfectant
solutions containing iodine. J Hosp Infect.
1985;6(Suppl A):1-11. [VA]
• National and state healthcare-associated infections
progress report. Atlanta (GA): National Center for
Emerging and Zoonotic Infectious Diseases, Centers
for Disease Control and Prevention; 2016
• Haley RW, Culver DH, White JW, Morgan WM,
Emori TG, Munn VP, et al. The efficacy of infection
surveillance and control programs
in preventing nosocomial infections in US hospitals.
Am J Epidemiol. 1985;121(2): 182-205.
• Naderi N, Maw K, Thomas M, Boyce DE, Shokrollahi
K. A quick and effective method of limb preparation
with health, safety and efficiency benefits. Ann R Coll
Surg Engl. 2012;94(2):83-86. [IIB]
• Incoll IW, Saravanja D, Thorvaldson KT, Small T.
Comparison of the effectiveness of painting onto the
hand and immersing the hand in a bag, in pre-operative
skin preparation of the hand. J Hand Surg Eur Vol.
2009;34(3):371-373. [IIB]
• Chou J, Choudhary A, Dhillon RS. Comparing sterile
bag rubbing and paint on technique in skin preparation
of the hands. ANZ J Surg. 2011;81(9):629-632. [IIC]
• Rodrigues AL, Simoes Mde L. Incidence of surgical
site infection with pre-operative skin preparation using
10% polyvidone-iodine and 0.5% chlorhexidine-
alcohol. Rev Col Bras Cir. 2013;40(6):443-8.
• Centers for Disease Control and Prevention. Guidelines
for evaluating surveillance systems. Morb Mortal Wkly
Rep (MMWR). 1988;37(5):1-18.
• Marchi M, Pan A, Gagliotti C, Morsillo F, Parenti M,
Resi D, et al. The Italian national surgical site infection
surveillance programme and its positive impact, 2009
to 2011. Euro Surveill. 2014;19(21): pii: 20815
http://www.who.int/gpsc/global-guidelines-web.pdf](https://image.slidesharecdn.com/otbasicguidelines-231018140809-9f604b5f/75/Opearation-theatre-Etiquette-76-2048.jpg)
