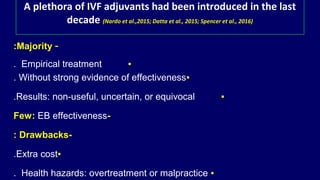
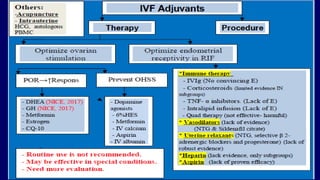
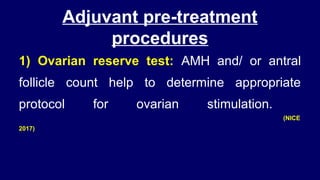
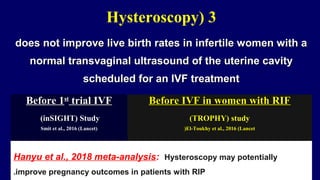
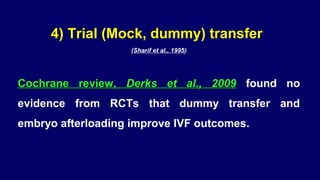
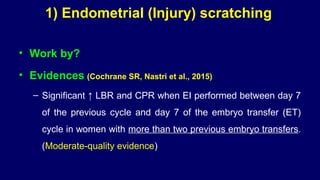
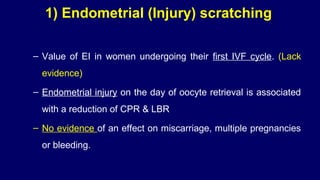
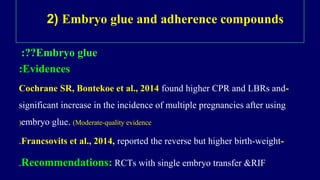
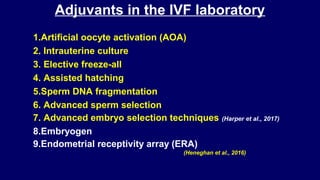
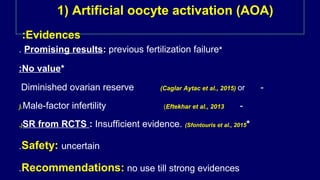
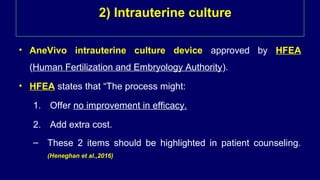
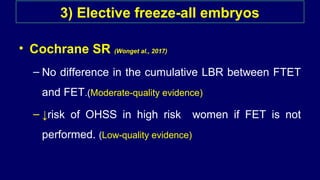
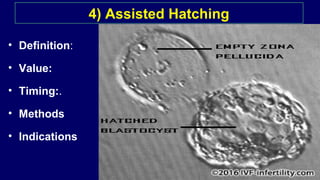
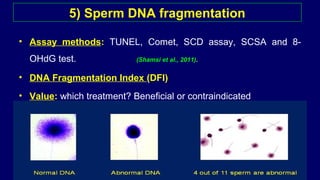
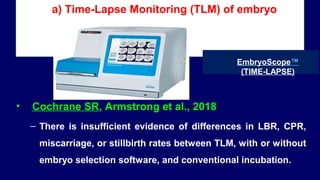
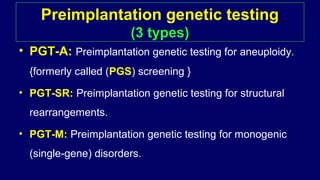
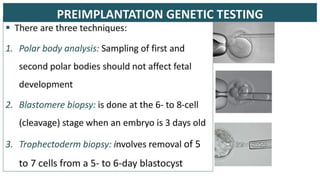
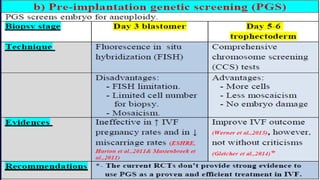
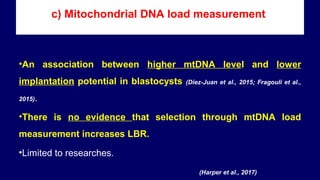
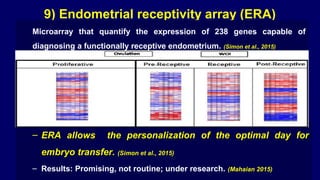
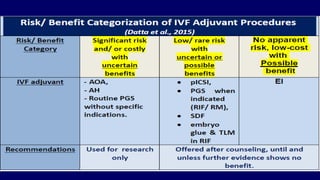
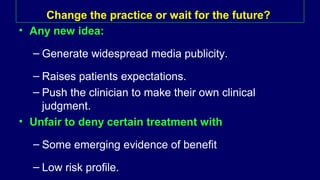
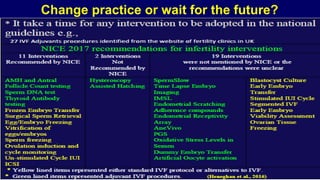
The document discusses the role and effectiveness of IVF adjuvants, which are optional treatments aimed at increasing live birth rates alongside standard IVF protocols. It highlights that many adjuvants lack strong evidence of efficacy, may incur additional costs, and could pose health risks. The conclusion emphasizes the need for high-quality randomized controlled trials before generalizing the use of these procedures in IVF clinics.