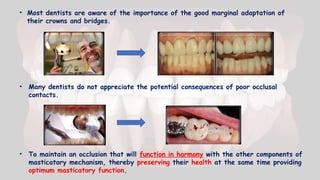
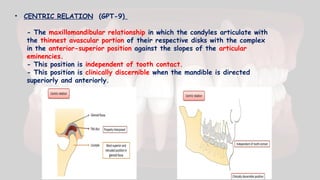
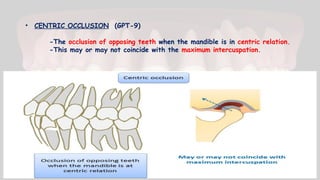
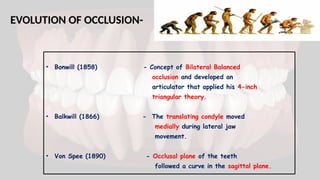
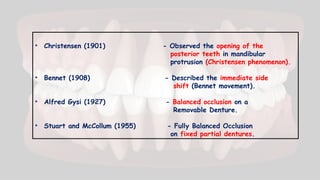
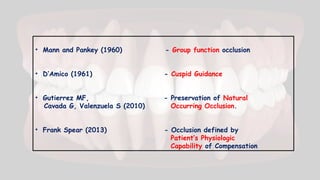
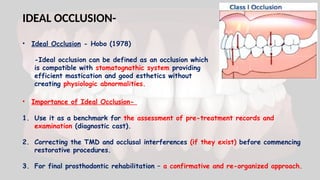
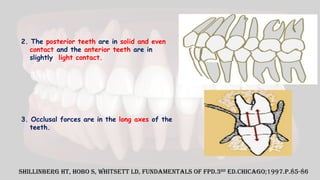
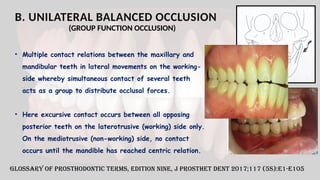
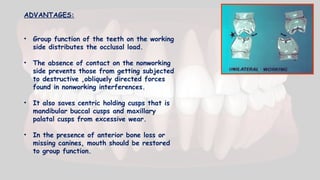
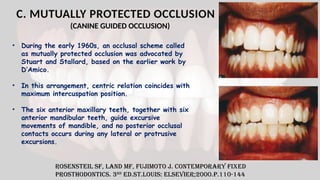
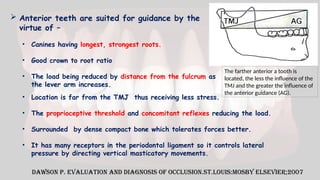
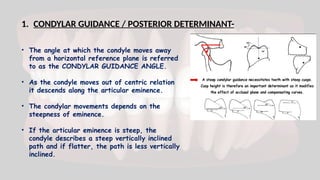
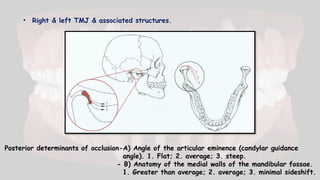
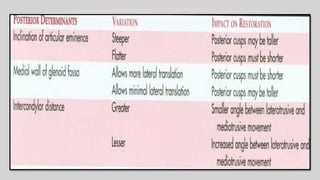
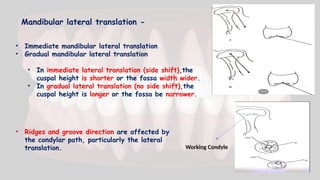
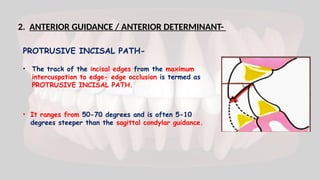
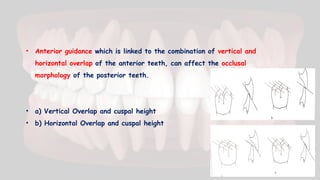
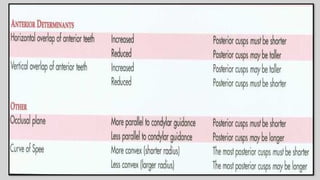
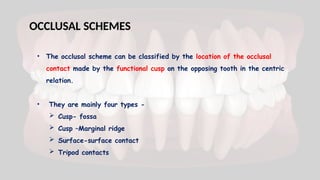
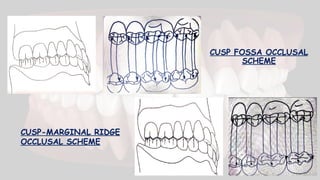
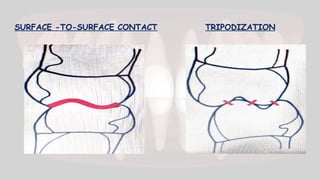
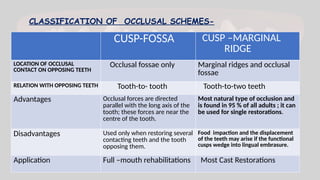
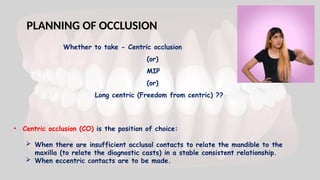
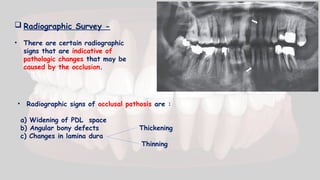
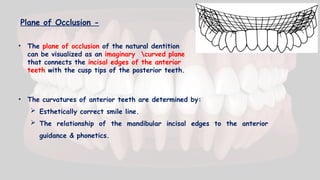
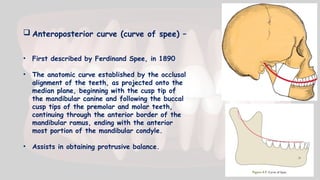
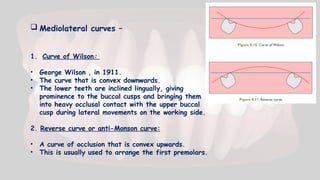
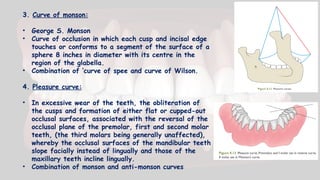
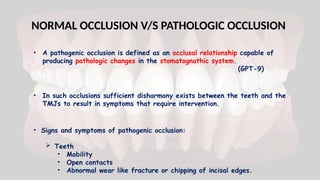
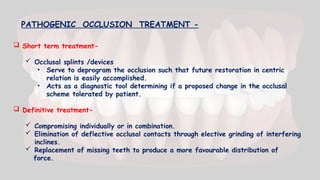
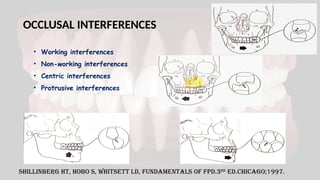
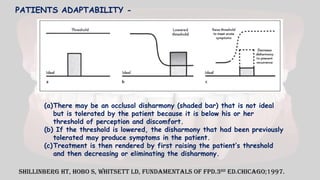
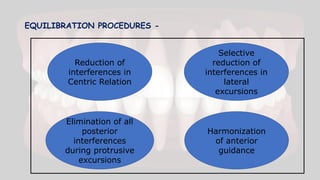
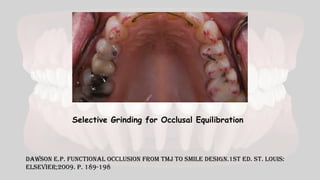
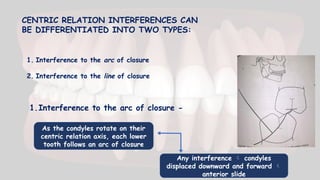
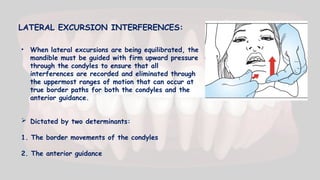
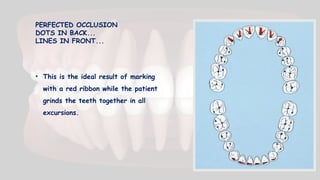
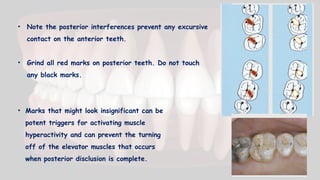
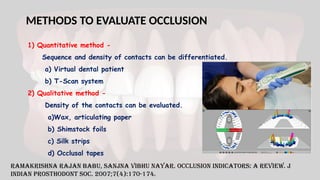
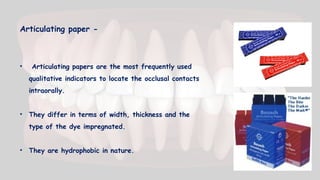
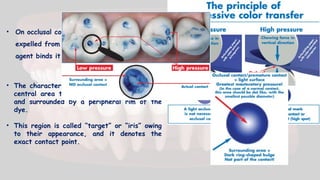
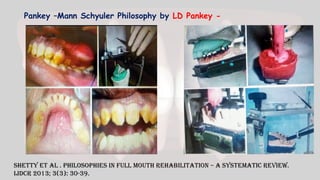
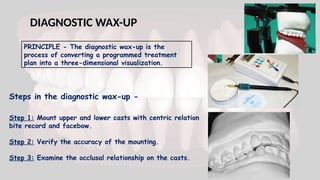
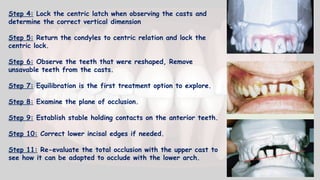
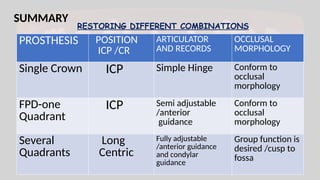
The document presents an in-depth exploration of occlusion in fixed partial dentures, emphasizing its importance for the long-term success of dental restorations and the maintenance of stomatognathic health. It covers the evolution of occlusion concepts, types of occlusion like ideal, optimal, and various occlusal schemes, while detailing occlusal determinants and methods for evaluation. Additionally, it describes factors such as centric occlusion, maximum intercuspation, and different occlusal contacts essential for effective dental treatment planning.