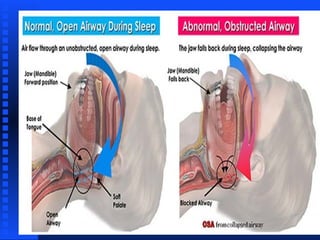
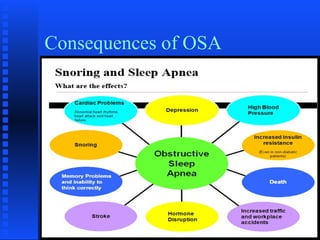
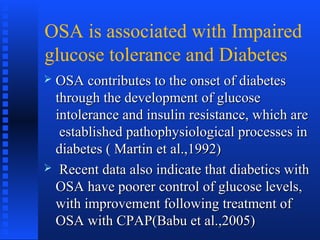
Obstructive sleep apnea (OSA) is a disorder where breathing is interrupted during sleep due to the airway becoming blocked or narrowed. It is characterized by pauses in breathing or instances of reduced breathing during sleep. A sleep study can be used to diagnose OSA by measuring the number of breathing pauses per hour. While weight loss and lifestyle changes are recommended, continuous positive airway pressure (CPAP) is the most effective treatment for OSA. Untreated OSA is associated with serious health risks like hypertension, cardiovascular disease, diabetes and stroke.











![Physical Exam
Height and Weight (BMI)Height and Weight (BMI)
BMI=[703.1 x weight(pounds)] / [Height (in)BMI=[703.1 x weight(pounds)] / [Height (in)22
]]
neck sizeneck size
Face-retrognathiaFace-retrognathia
NoseNose
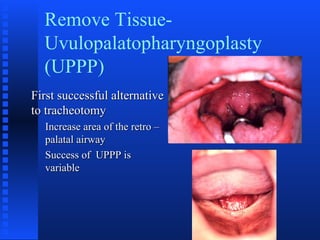
Oral cavity- palate, uvula, tonsils/pillars,Oral cavity- palate, uvula, tonsils/pillars,
tongue, occlusiontongue, occlusion](https://image.slidesharecdn.com/obstructivesleepapnea-180114105619/85/Obstructive-sleep-apnea-18-320.jpg)