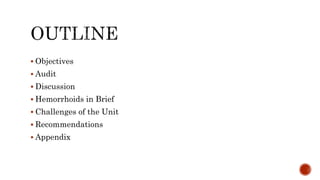
The document summarizes a gastroenterology audit conducted at SPHMMC in November 2018. 57 colonoscopies were performed and data was collected on patient demographics, indications for procedures, findings, and challenges. The most common indications were ruling out colorectal cancer (26.3%) and lower GI bleeding (14%). The most common findings were normal (28%), hemorrhoids (22.8%), and colorectal carcinoma (14%). Opportunities for improvement included standardizing report formats, assessing bowel prep quality, and monitoring key performance indicators like adenoma detection rates.
![Beka Aberra [R2]
SPHMMC Gastroenterology Attachment
Moderator: Yemiserach Chane, MD, Internist/Gastroenterologist
December, 2018](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-1-320.jpg)
![Data resources
Colonoscopy Report Papers from November 1- 30 or
From [Tikemt 22 -Hidar 21]
In the Month of November 57Colonoscopies were done.
Colonoscopy Audit.xlsx](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-4-320.jpg)
![NUMBER PERCENTAGE
GENDER MALE 31 56.3%
FEMALE 24 43.6%
AGE GROUPS
* < 40 yrs were[18]
* >= 40 yrs were [37]
0-9 0 0%
10-19 1 1.8%
20-29 12 21.8%
30-39 5 9%
40-49 10 18.3%
50-59 15 27.3%
60-69 5 9%
70-79 6 11%
80-89 1 1.8%
Patients were Aged between [18-85 years] with Mean Age 46.42 Years;
56.3% Males and 43.6% Females](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-5-320.jpg)
![0%
5%
10%
15%
20%
25%
30%
0
2
4
6
8
10
12
14
16
0-9 [10-19] [20-29] [30-39] [40-49] [50-59] [60-69] [70-79] [80-89]
AGE GROUPS
Chart Title
NUMBER PERCENTAGE](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-6-320.jpg)
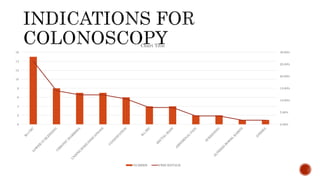
![INDICATIONS NUMBER PERCENTAGE
R/o CRC 15 26.30%
LOWER GI BLEEDING 8 14%
CHRONIC DIARRHEA 7 12.30%
UNSPECIFIED INDICATIONS 7 12.30%
CONSTIPATION 6 10.60%
R/o IBD 4 7%
RECTAL MASS 4 7%
ABDOMINAL PAIN 2 3.50%
SCREENING 2 3.50%
ALTERED BOWEL HABITS 1 1.75%
ANEMIA 1 1.75%
The Commonest Indications
being Rule Out CRC [26.3%]
followed by LGIB [14%].](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-7-320.jpg)
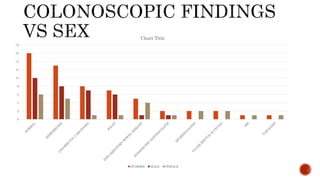
![DIAGNOSIS NUMBER PERCENTAGE MALE FEMALE
NORMAL 16 28% 10 6
HEMORROIDS 13 22.80% 8 5
COLORECTAL CARCINOMA 8 14% 7 1
POLYP 7 12.20% 6 1
INFLAMMATORY BOWEL DISEASE 5 9% 1 4
NONSPECIFIC ILEITIS/COLITIS 2 3.50% 1 1
DIVERTICULOSIS 2 3.50% 0 2
ULCER [RECTAL & CECAL] 2 3.50% 0 2
IBS 1 1.75% 0 1
TAENIASIS 1 1.75% 0 1](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-9-320.jpg)
![0%
5%
10%
15%
20%
25%
30%
0
2
4
6
8
10
12
14
16
18
Normal Hemorroids Colorectal Cancer Polyps IBD Nonspecific
Ileitis/Colitis
Ulcer
[Rectal/Cecal]
Diverticulosis IBS Taeniasis
Chart Title
Frequency Percent
Diagnostic yield is about 72% for colonoscopy of the
Total Indications [57]; Normal Findings were [16].
53 % for CRC [15 R/o CRC Indications; 8 Findings]
62.5% for Hemorrhoids [8 LGIB Indication; 5H/3P]](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-10-320.jpg)
![FINDINGS NORMAL HEMORRHOIDS CRC POLYPS IBD NONSPECIFIC
ILEITIS/
COLITIS
DIVERTICUL
OSIS
ULCER
[RECTAL/
CECAL]
IBS TAENIASI
S
AGE
GROUPS
0-9 0
0 0 0 0 0 0 0 0 0
10-19 0
0 0 0 0 0 0 0 0 1
20-29 3 2 2 1 3 0 0 0 1 0
30-39 0
2 0 0 0 0 1 2 0 0
40-49 3
2 2 1 1 0 1 0 0 0
50-59 7 1 3 2 0 2 0 0 0 0
60-69 0
3 0 2 0 0 0 0 0 0
70-79 3
2 1 0 0 0 0 0 0 0
80-89 0
0 0 1 0 0 0 0 0 0](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-12-320.jpg)
![ Polyp Detection Rate Calculation Method: # of colonoscopy cases with at least one
polyp was biopsied or removed/Total # of screening colonoscopies.
Polyps 7/57 [12.3%] vs CRC 8/57 [14%]
FINDINGS NORMAL CRC POLYPS
AGE GROUPS
* < 40 yrs were[2/1]
* >= 40 yrs were [6/6]
***Above Age of 40 yrs Fecal
Occult Blood testing +
DRE/Endoscopic Exams may
be necessary
0-9 0
0 0
10-19 0
0 0
20-29 3 2 1
30-39 0
0 0
40-49 3
2 1
50-59 7 3 2
60-69 0
0 2
70-79 3
1 0
80-89 0
0 1](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-21-320.jpg)
![Non Operative/Office procedures
Sclerotherapy
Band Ligation
Infra-red coagulation
Cryosurgery
Manual dilatation of anus
Sphicterotomy [Lateral]
Bicap Electrocoagulation
Haemorrhoidolysis](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-49-320.jpg)

![Operative Hemorrhoidectomy
Milligan-Morgan Hemorrhoidectomy [OPEN]
Ferguson’s Hemorrhoidectomy [CLOSED]](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-54-320.jpg)
![ Scope Problems
Screening the patients Diagnostic yield was only 72 %.
Different Colonoscopic reporting formats used
Many Incomplete data fillings; Mostly Duration of procedure.
Lack of Standard Grading of Bowel Preparation [BBPS].
Lack of Imaging of Findings.
Less therapeutic activities done; Mostly Diagnostic.
No strict follow-up of patients post colonoscopy for complication detection.](https://image.slidesharecdn.com/colonoscopy2-190116142321/85/Hemorrhoids-Colonoscopy-Audit-57-320.jpg)