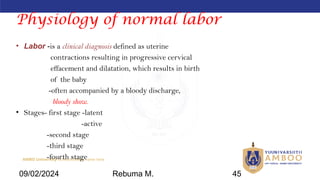
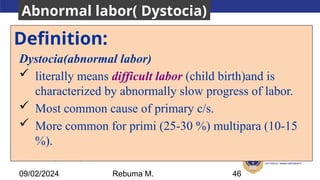
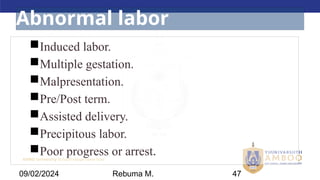
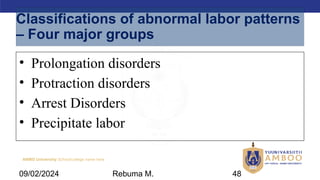
The document focuses on the concepts of analgesia and anesthesia in obstetric care, detailing their definitions and importance in pain relief during labor. It discusses the anatomical and hormonal factors that influence labor and the various methods and techniques for pain management, including regional anesthesia types and their applications. Additionally, it outlines complications associated with anesthesia during cesarean sections and the classification of abnormal labor patterns and their management.


![AMBO University School/college name here
I. Interactive presentation, case scenario [6hr]
1. Anesthesia and Analgesics (2hrs)
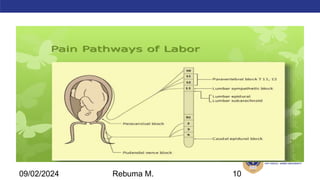
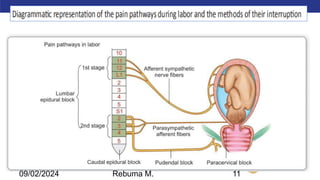
• Review mechanism of pain
• Introduction
• Type
• Complications /side effects
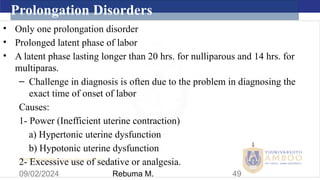
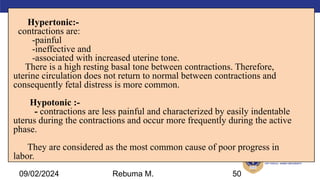
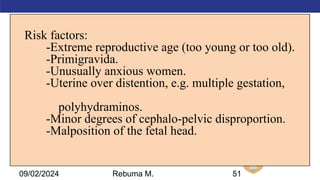
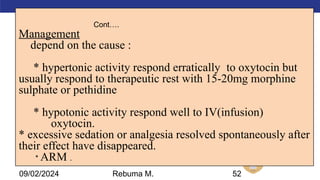
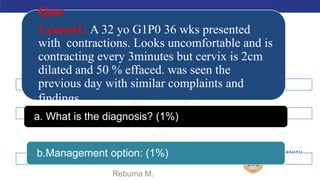
2. Abnormal labor [4hrs]
Prolonged latent phase
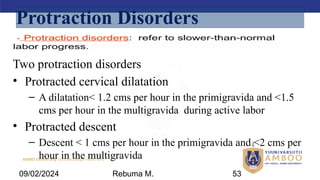
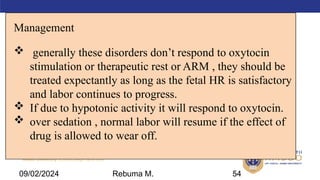
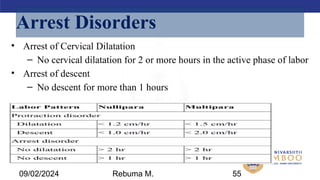
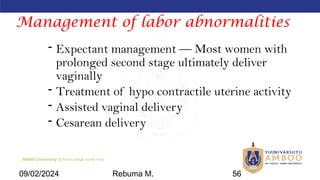
Protraction and arrest disorders
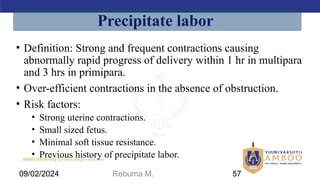
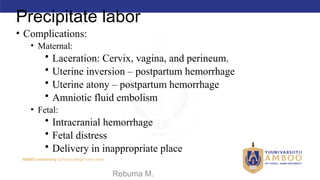
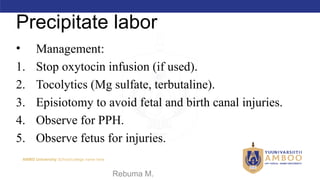
Precipitate labor
Skill Development Lab [3hrs]
Prepare and administer medications (Demonstration)
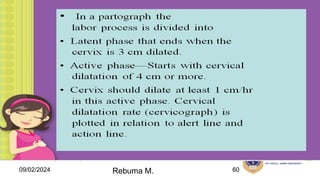
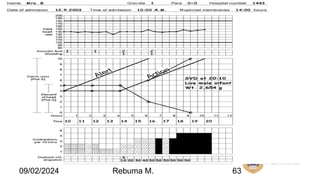
Abnormal progress of labor (video, interpreting partograph)
PBL [4hrs]
Abnormal labor
09/02/2024 Rebuma M. 121](https://image.slidesharecdn.com/obsiiclasshandout-240902172901-13beef99/85/obstetrics-II-class-handout-pptx-121-320.jpg)
![AMBO University School/college name here
II. Interactive presentation, case scenario [6hrs.]
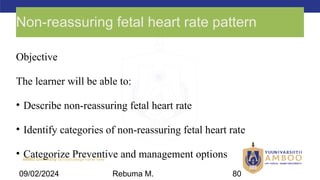
3. Non-reassuring fetal heart rate pattern [2hr]
Introduction
Pathophysiology
Cause
Care and management
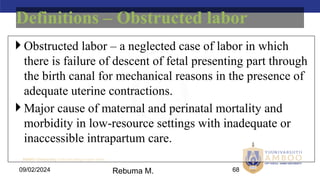
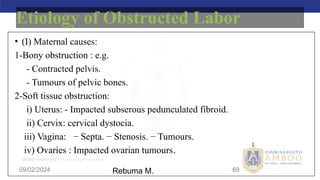
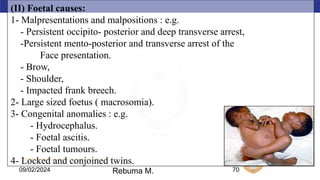
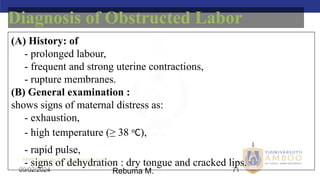
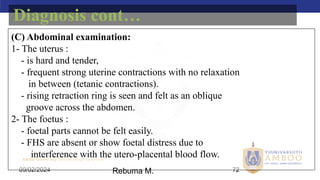
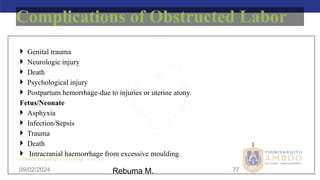
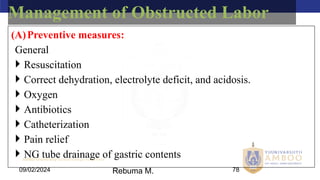
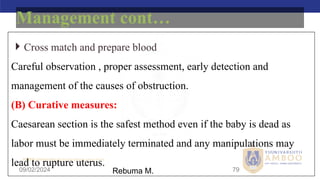
4. Obstructed labor [2hr]
Introduction
Risk factors and causes
Care and management
Skill Development Lab [2hrs]
Cephalopelvic disproportion & obstructed labor
PBL [4hrs]
Obstructed labor
Non-reassuring fetal heart rate pattern
09/02/2024 Rebuma M. 122](https://image.slidesharecdn.com/obsiiclasshandout-240902172901-13beef99/85/obstetrics-II-class-handout-pptx-122-320.jpg)
![AMBO University School/college name here
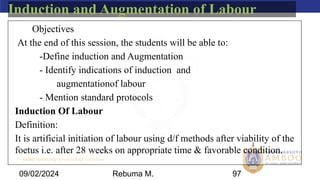
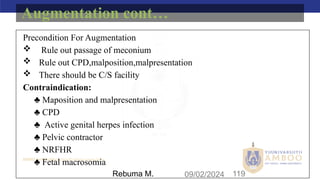
5. Induction and Augmentation of labor [2hrs]
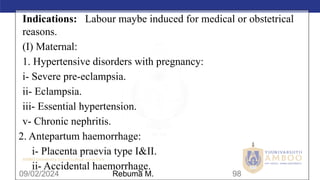
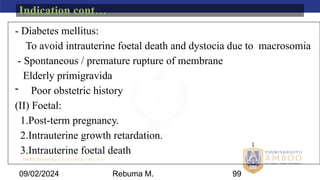
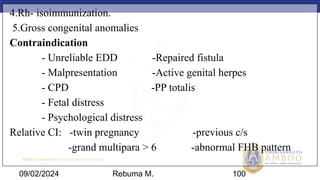
Indications for induction and augmentation
Contraindications for induction and augmentation](https://image.slidesharecdn.com/obsiiclasshandout-240902172901-13beef99/85/obstetrics-II-class-handout-pptx-123-320.jpg)