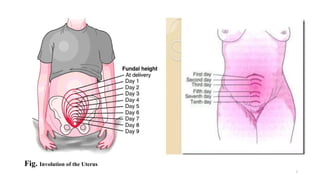
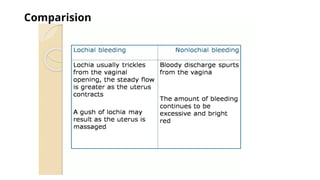
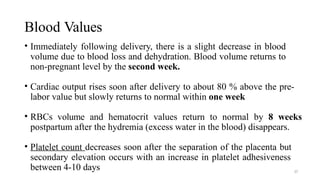
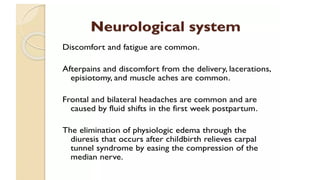
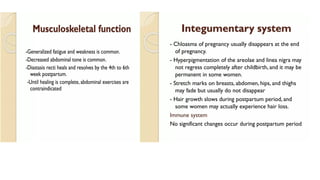
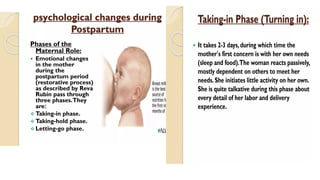
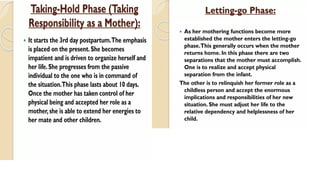
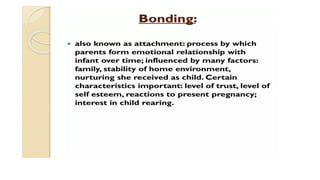
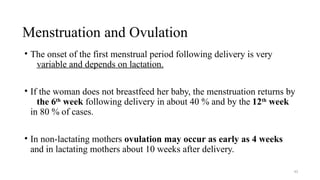
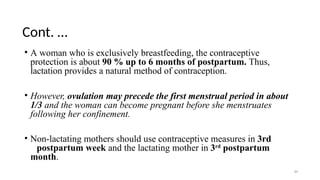
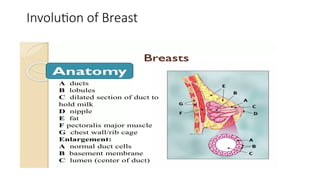
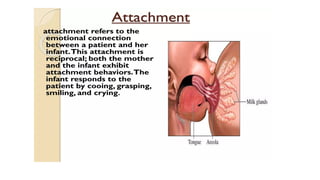
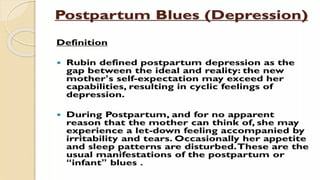
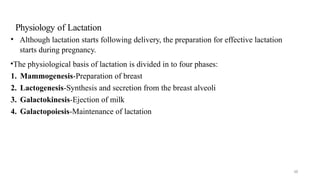
The document outlines the normal puerperium period following childbirth, detailing physiological and anatomical changes in the body as it returns to prepregnant status over approximately six weeks. It describes stages of involution, changes in reproductive organs, the characteristics and significance of lochia, and adjustments in other bodily systems. Additionally, it highlights the emotional changes and the implications of breastfeeding on hormonal levels and menstrual cycles.