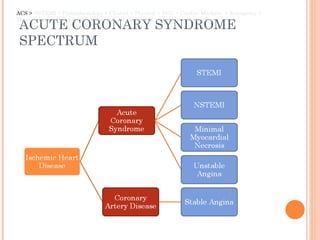
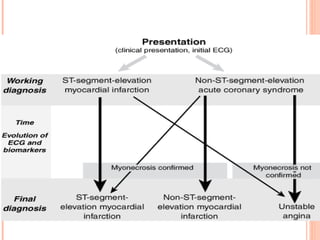
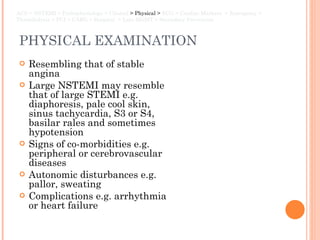
The document discusses non-ST elevation myocardial infarction (NSTEMI), including its pathophysiology, clinical presentation, diagnostic testing, and management. NSTEMI is caused by reduced blood supply or increased oxygen demand in the heart muscle due to atherosclerotic plaque. Patients experience chest pain and may have abnormal ECG or elevated cardiac enzymes. Treatment involves aspirin, anticoagulants, reperfusion therapies like thrombolysis or angioplasty, and long-term secondary prevention including medications and lifestyle changes.


















![EMERGENCY MANAGEMENT ABC, Pulse Oximeter, Attach ECG monitor and record 12-lead ECG, High flow O2 by face mask IV access [bloods for CBC, U&E, glucose, lipids, cardiac enzymes] Brief assessment History of CVS disease, risk factors for IHD Examination: pulse, BP, JVP, cardiac murmurs, scar from previous cardiac surgery Aspirin 300 mg or Clopidogrel 75mg Morphine 5-10 mg IV + metoclopramide 1 mg IV GTN sublingually Thrombolysis management Beta blockers + ACEI ACS > NSTEMI > Pathophysiology > Clinical > Physical > ECG > Cardiac Markers > Emergency > Thrombolysis > PCI > CABG > Hospital > Late MGMT > Secondary Prevention](https://image.slidesharecdn.com/nstemi-hafiz-120208011111-phpapp01/85/NSTEMI-DrHafiz-23-320.jpg)