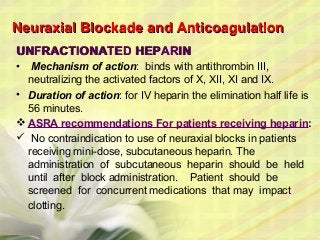
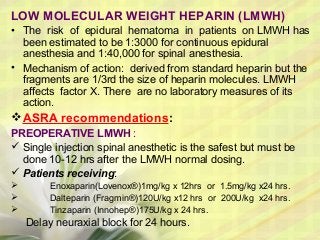
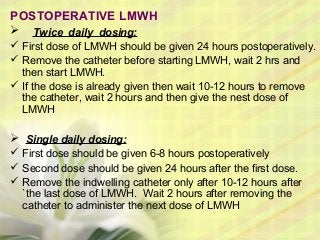
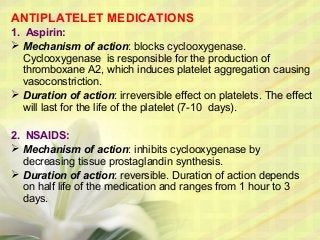
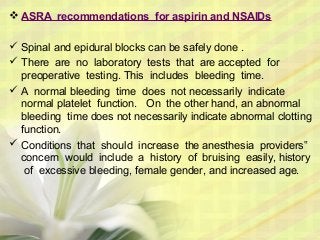
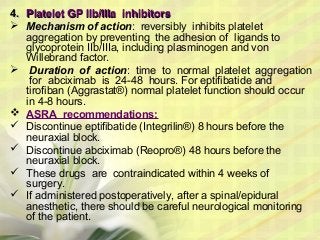
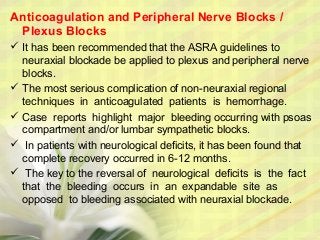
This document discusses anticoagulation and neuraxial anesthesia. It begins by introducing some risks of anticoagulation like bleeding. It then focuses on the risks of spinal and epidural hematoma formation during regional anesthesia when patients are anticoagulated. It provides recommendations from ASRA on the timing of regional blocks for various anticoagulants like heparin, LMWH, warfarin, antiplatelets, and newer anticoagulants. It also briefly discusses peripheral nerve blocks and herbal therapies. The recommendations aim to balance thrombosis prevention with bleeding risks from regional anesthesia.