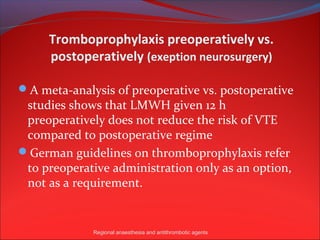
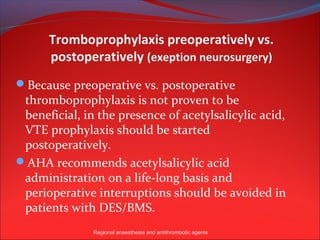
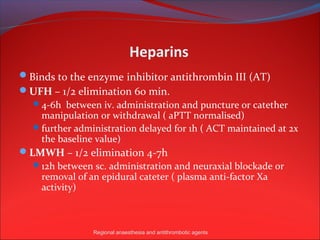
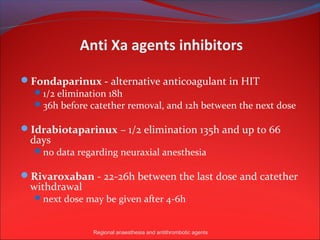
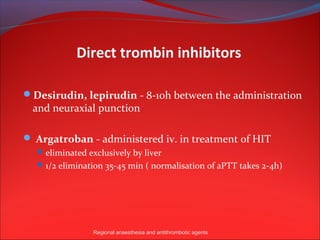
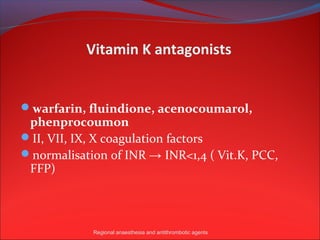
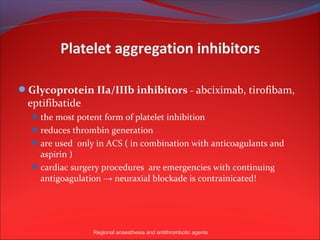
The document summarizes the 2010 recommendations of the European Society of Anesthesiology on neuraxial anesthesia and antithrombotic drugs. It provides time intervals that should elapse between taking different antithrombotic medications and performing neuraxial blocks or catheter removals based on the half-lives of the drugs. It also discusses preoperative versus postoperative thromboprophylaxis and considerations for various classes of antithrombotic agents including heparins, anti-Xa agents, direct thrombin inhibitors, vitamin K antagonists, and platelet aggregation inhibitors.