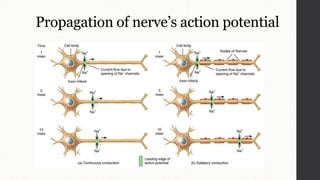
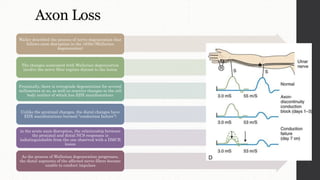
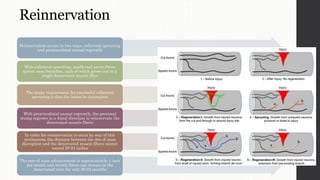
Nerve conduction studies (NCS) involve stimulating peripheral nerves and recording the electrical responses in muscles or other nerves. NCS can localize lesions to specific locations (e.g. root, plexus) and characterize the pathology (e.g. demyelination, axon loss). For motor NCS, responses are recorded from muscles. Sensory NCS records small responses from nerves. Demyelination and axon loss can be detected based on changes in latency, conduction velocity and response amplitude. Wallerian degeneration occurs distally after axon disruption and impacts NCS results over time. Reinnervation of muscles can occur through collateral sprouting or axon regrowth.

![Introduction
The electrodiagnostic (EDX)
examination is an extension of
the clinical neurologic
examination that provides
important information about the
peripheral nervous system (PNS)
EDX testing of the PNS includes
nerve conduction studies (NCSs),
the needle electrode examination
(NEE)
The two major goals of the EDX
examination include lesion
localization (root, plexus, nerve,
neuromuscular junction [NMJ],
muscle) and lesion
characterization
(pathophysiologic features,
severity, and rate of progression)
It’s not only of diagnostic utility,
but it also contributes to patient
management and prognosis](https://image.slidesharecdn.com/nerveconductionstudyncs-210915173729/85/Nerve-conduction-study-ncs-2-320.jpg)