This document outlines neonatal sepsis, including:
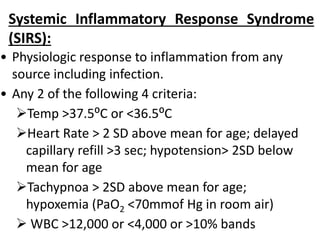
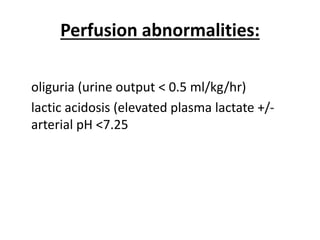
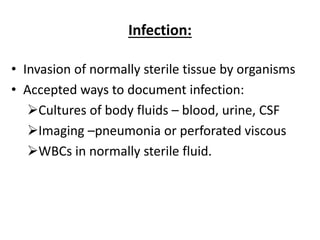
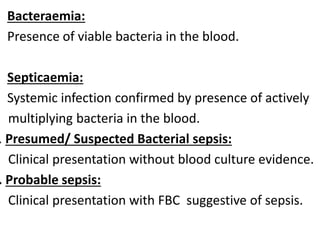
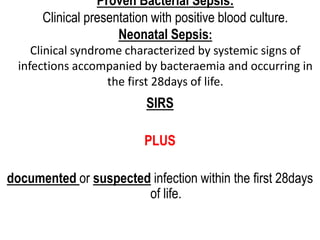
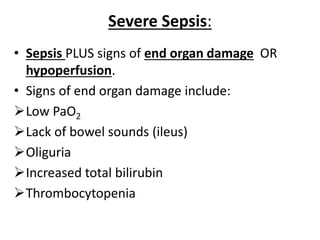
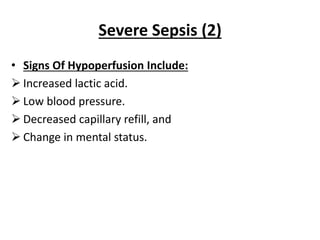
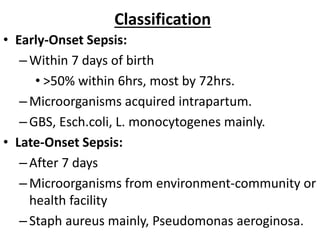
- It defines terms like sepsis, severe sepsis, and septic shock.
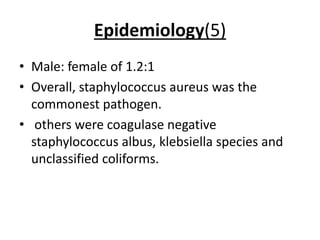
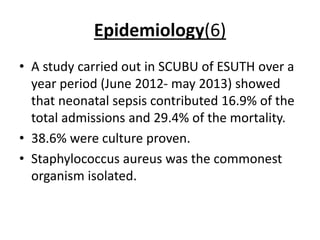
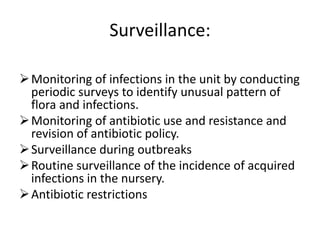
- Epidemiology shows it is one of the top causes of NICU admission and mortality, with incidence varying globally.
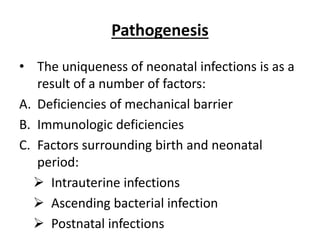
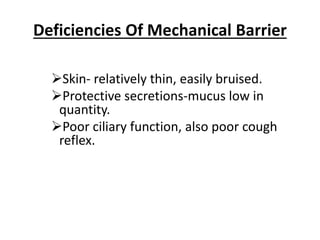
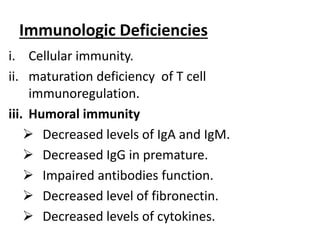
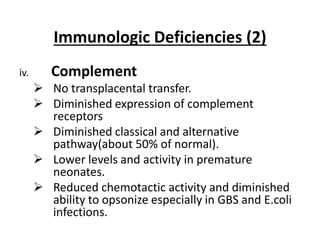
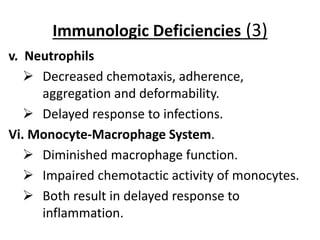
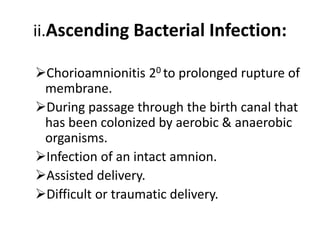
- Pathogenesis is explained by neonates' immature immune systems and barriers to infection.
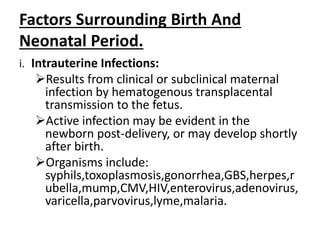
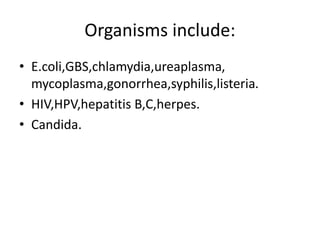
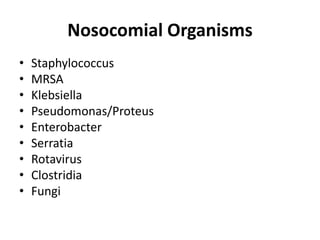
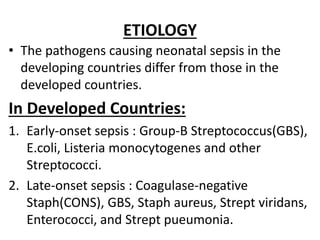
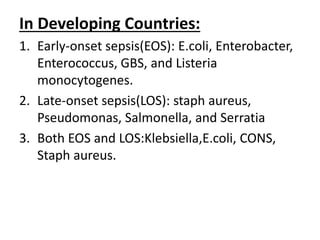
- Etiology differs between developing and developed countries.
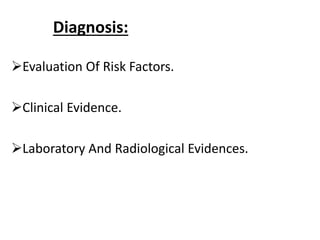
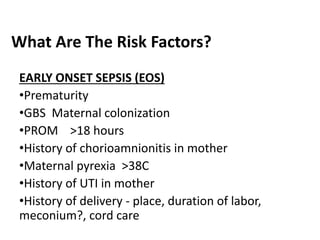
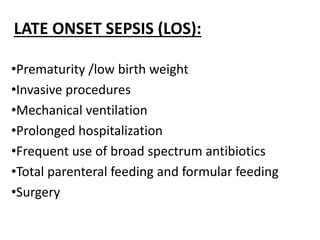
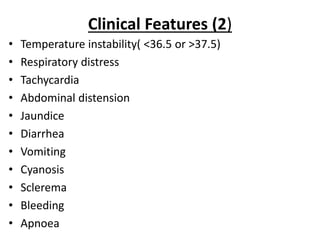
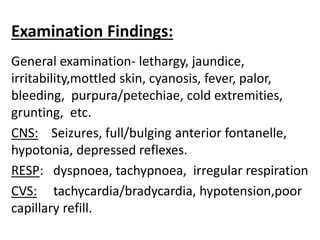
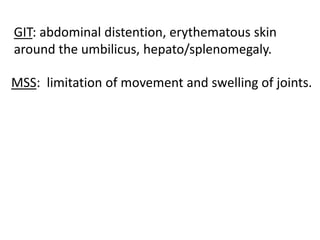
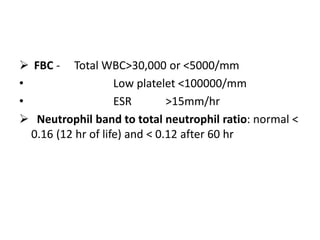
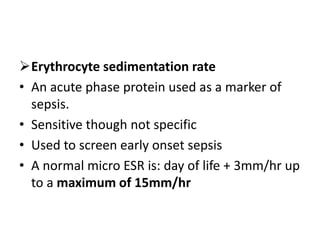
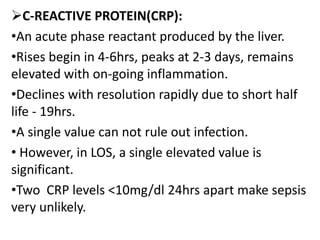
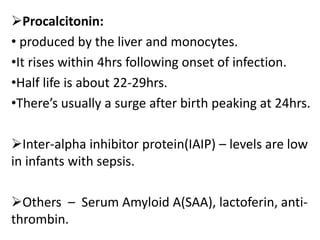
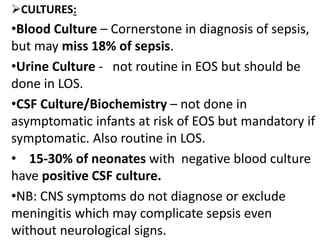
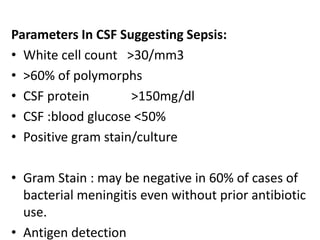
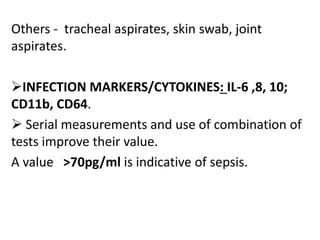
- Diagnosis involves clinical evaluation, labs like blood counts and cultures, and radiology when needed.
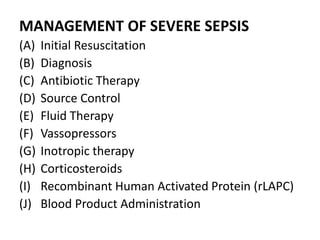
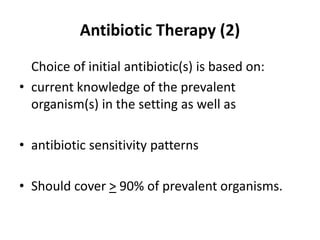
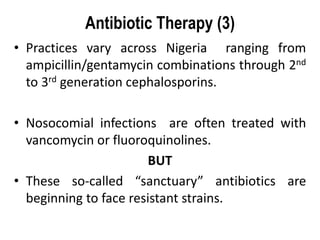
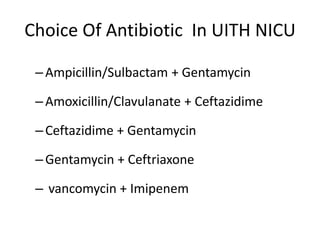
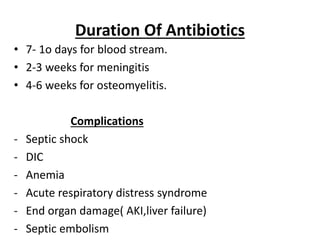
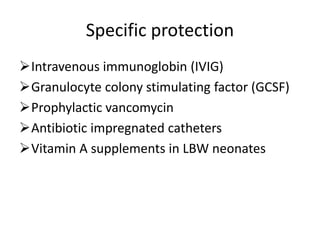
- Management involves cultures, antibiotics, fluid resuscitation, inotropes, and source control as needed for severe cases.