This document discusses neonatal sepsis, including:
- Definition, epidemiology, pathogenesis, predisposing factors, etiology, classification, clinical symptoms, investigations, evaluation, management, supportive measures, antibiotics used, complications, prevention, and questions.
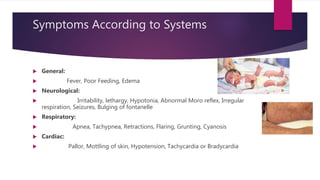
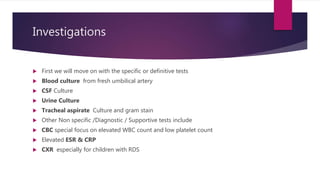
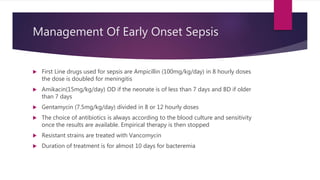
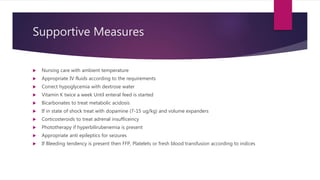
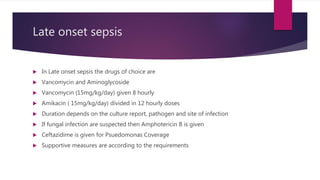
Neonatal sepsis is defined as a clinical syndrome resulting from infection in newborns. It can be early onset (within 3 days of life) or late onset (4 days to 1 month). Common causes are E. coli, Klebsiella, GBS. Management involves early recognition, supportive care, and appropriate antibiotic therapy based on culture results. Outcomes can be improved with prompt diagnosis and treatment.