1. Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection that is an important cause of morbidity and mortality in newborns.
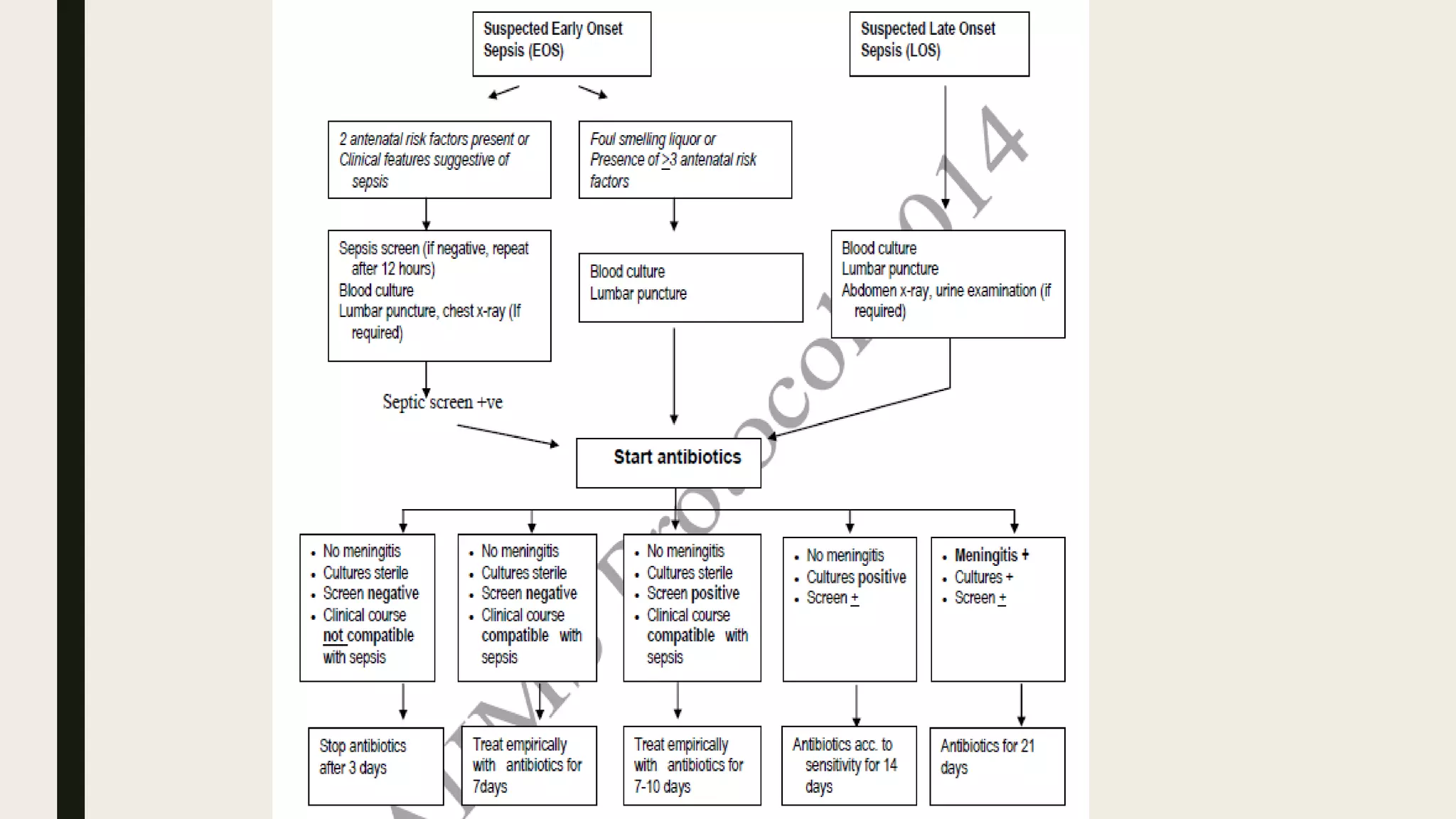
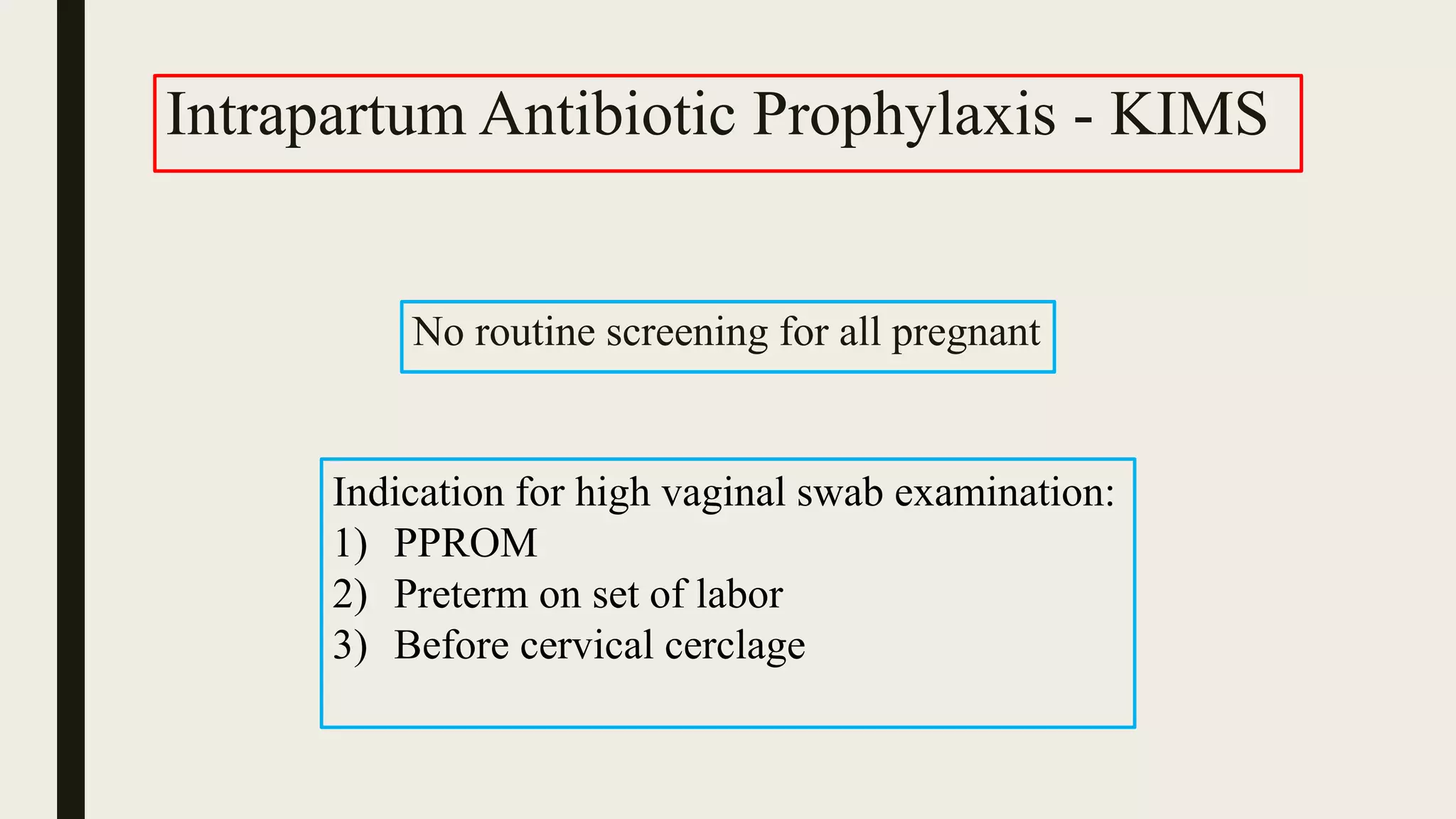
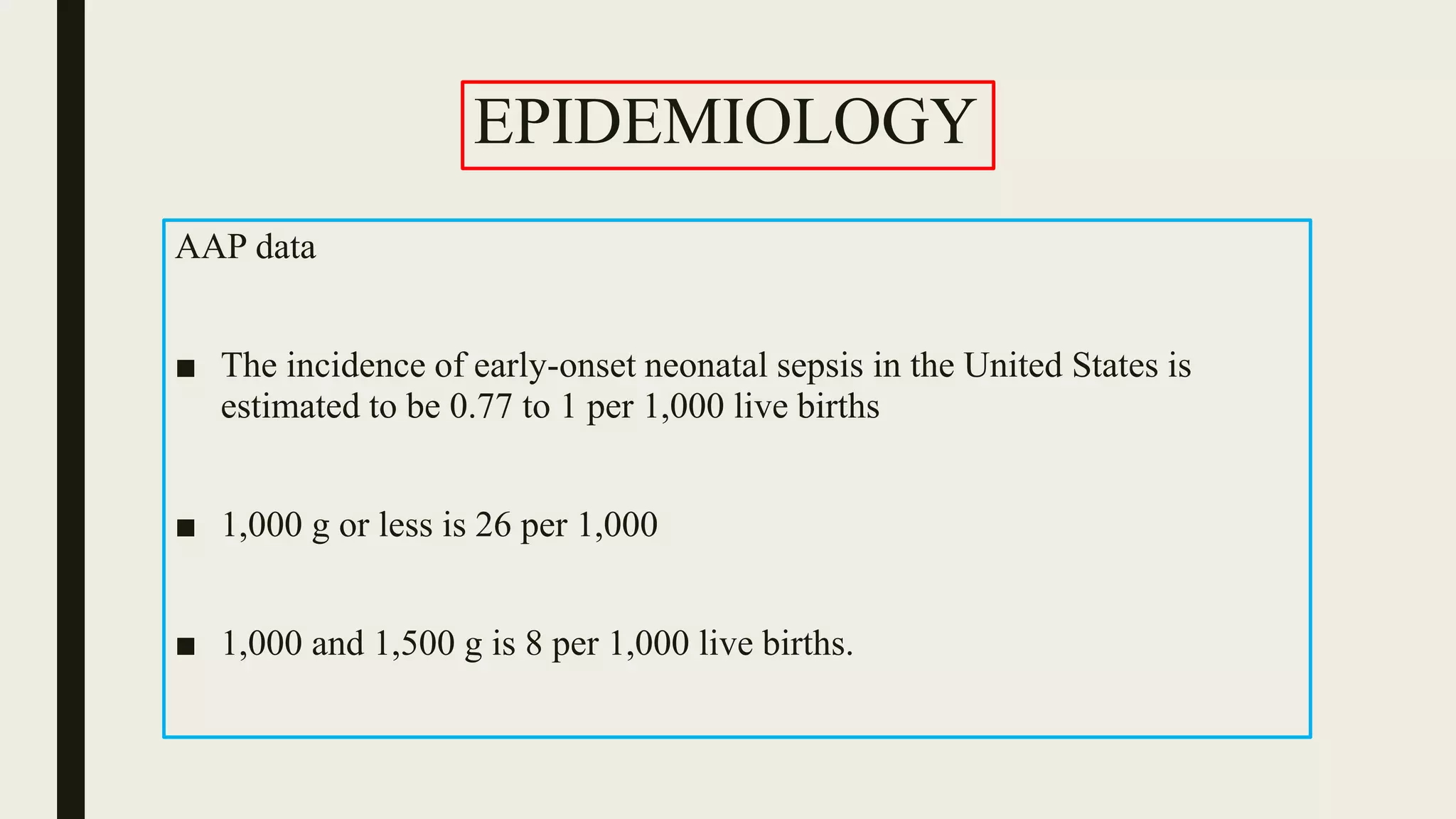
2. The document outlines risk factors, screening protocols, common pathogens, and empirical antibiotic protocols for treating early-onset neonatal sepsis at KIMS hospital in India.
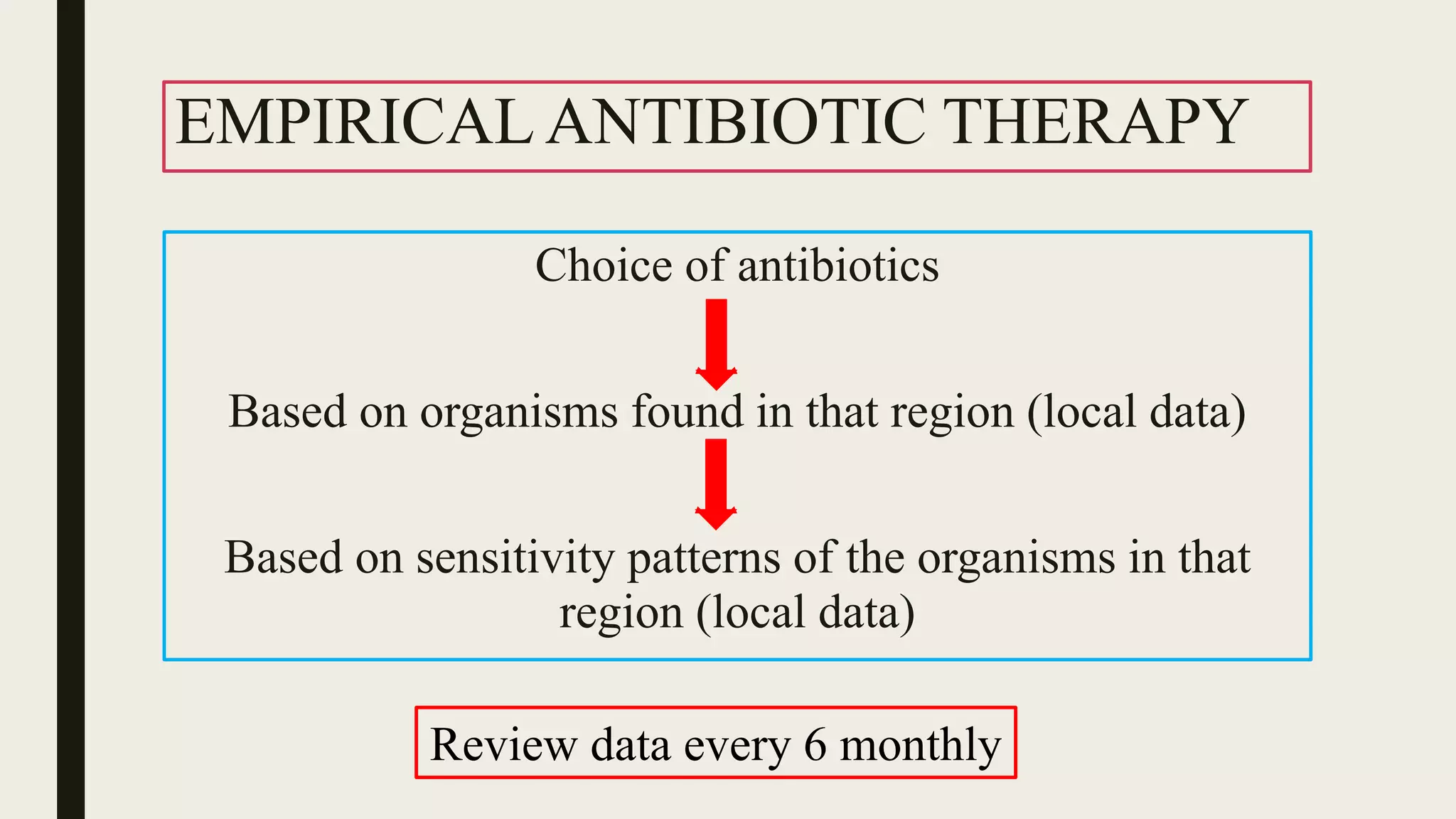
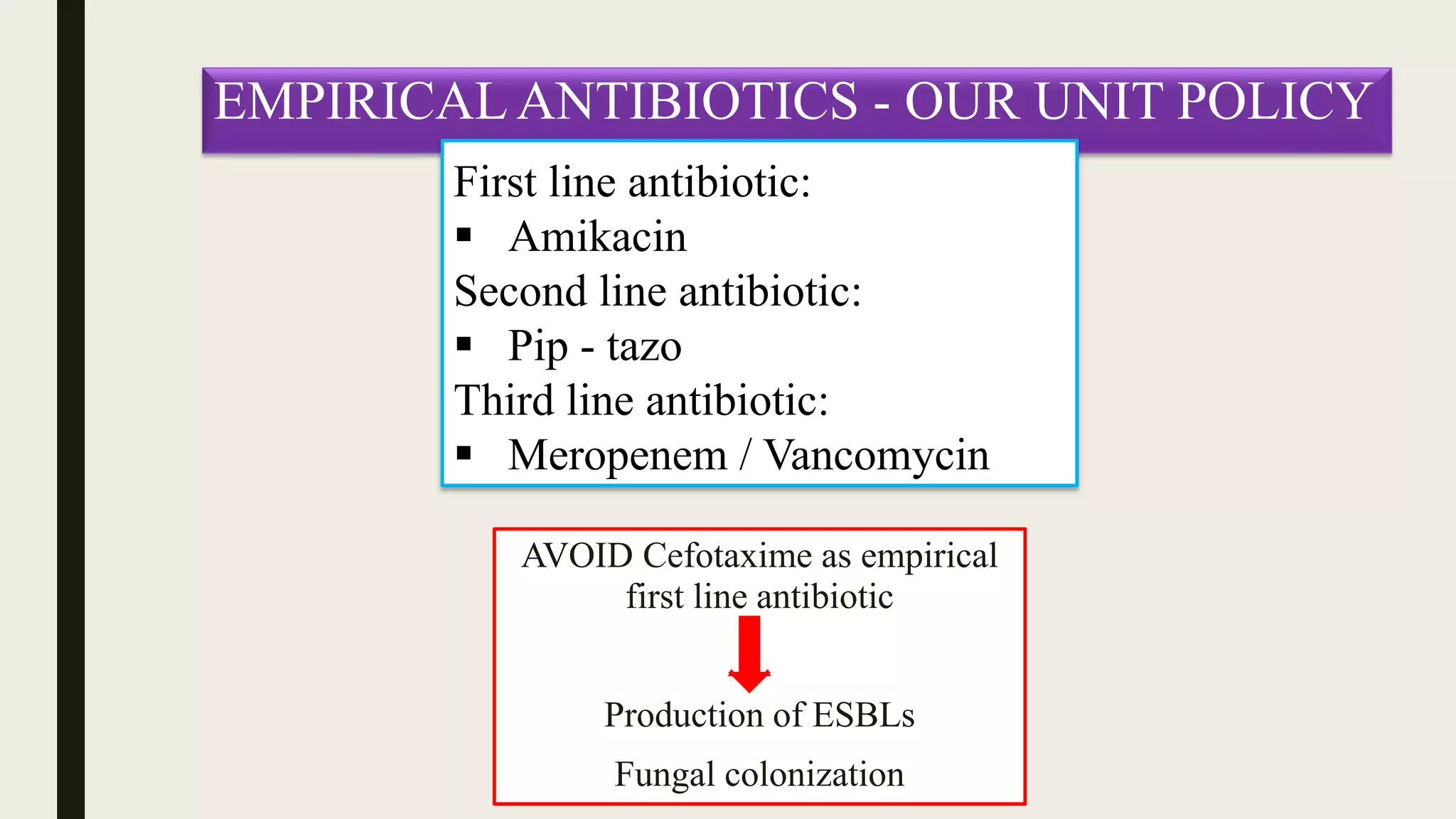
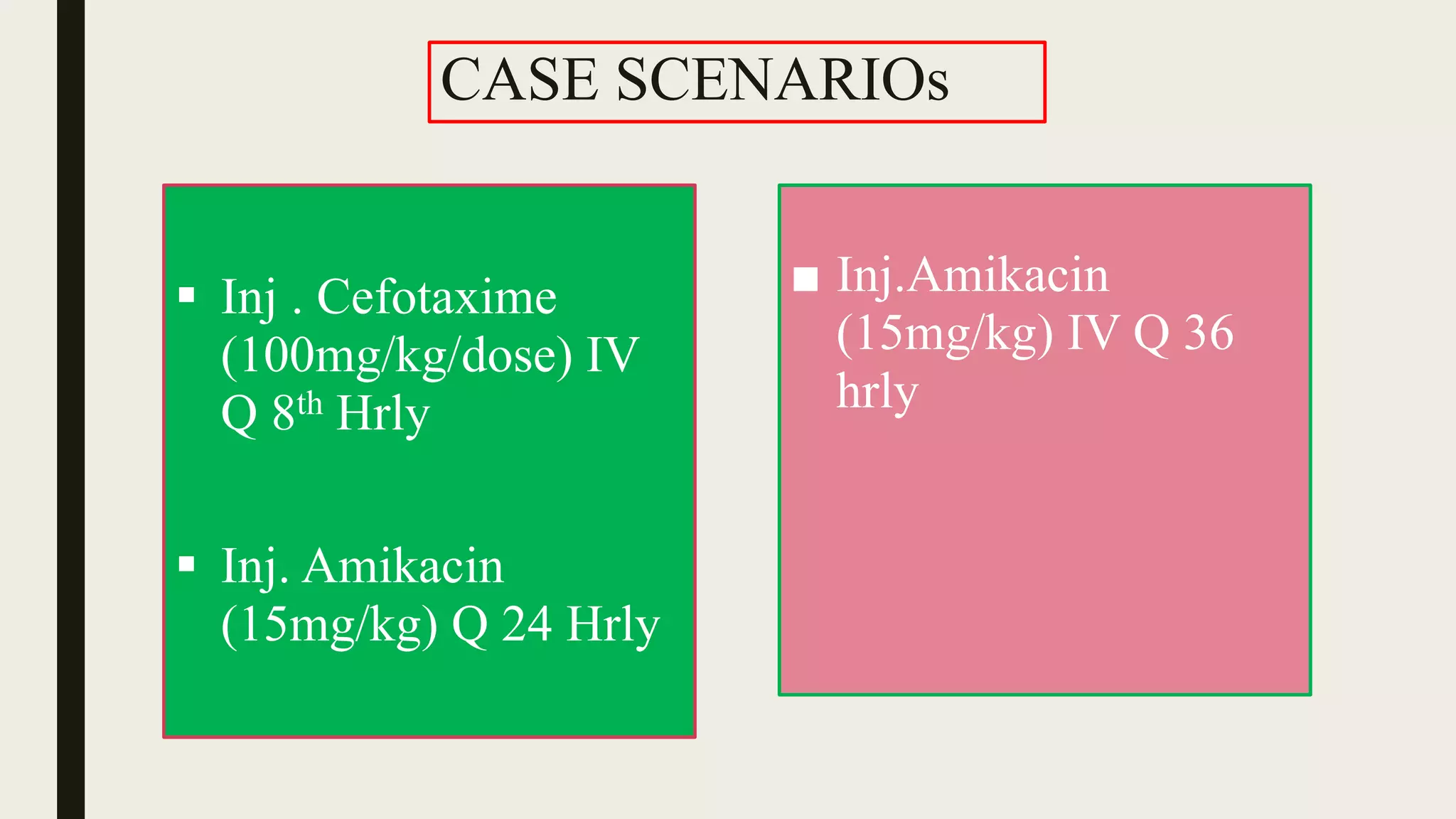
3. Based on local data, the first-line empirical antibiotic recommended for treating suspected early-onset neonatal sepsis at KIMS is amikacin, with pip-tazo as second-line and meropenem or vancomycin as third-line options.














![Definition of chorioamnionitis?
Clinical signs and symptoms of chorioamnionitis include:
1. Fever: T > 101 º F (38.3 º C) at any time or intrapartum T >100.4 º F
(>37.8 º C) twice, more than 1 hour apart
2. Maternal tachycardia (>100-120 beats per minute [bpm])
3. Fetal tachycardia (>160-180 bpm)
4. Purulent or foul-smelling amniotic fluid/vaginal discharge
5. Uterine fundal tenderness
6. Maternal leukocytosis (total >15,000-18,000 cells/μL)](https://image.slidesharecdn.com/neonatalsepsisppt-180220072454/75/Neonatal-sepsis-protocols-21-2048.jpg)