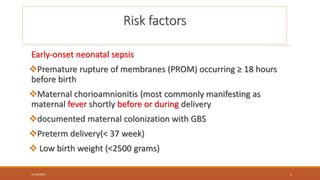
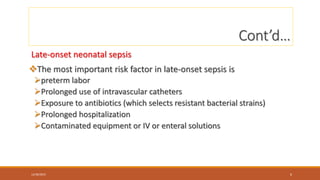
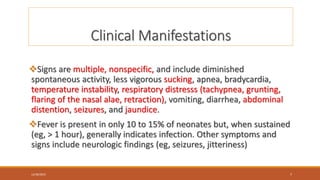
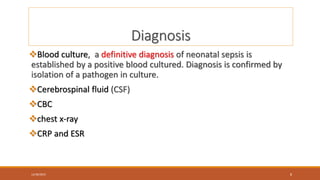
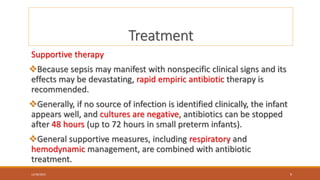
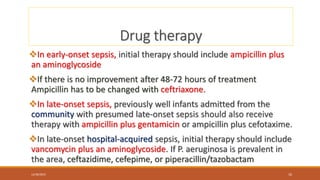
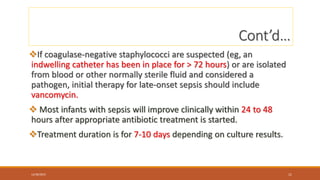
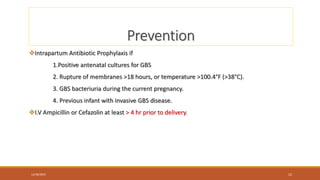
Neonatal sepsis is an invasive infection that usually occurs during the neonatal period. It is classified as either early-onset sepsis (presenting within 72 hours of life) or late-onset sepsis (presenting after 72 hours of life). Early-onset sepsis is generally caused by group B streptococcus or gram-negative bacteria from the maternal genital tract. Late-onset sepsis is usually hospital-acquired and caused by staphylococci or other nosocomial pathogens. Risk factors include prematurity, prolonged rupture of membranes, and prolonged hospitalization. Treatment involves supportive care and empiric antibiotics, with initial therapy dependent on the suspected causative organism and timing of onset. Prevention strategies focus on intrapartum antibiotic pro