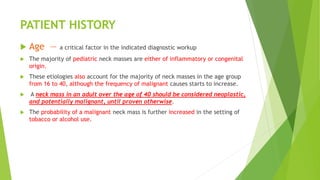
This document provides guidelines for evaluating neck masses. It discusses obtaining a thorough patient history, including details on mass growth, symptoms, medical history and social history. Physical examination involves carefully examining the mass characteristics and location. Important investigations include a complete blood count, inflammation markers, specific infection serologies depending on risk factors, and contrast CT scan of the neck, which is usually the initial preferred imaging study. Fine needle aspiration may be guided by ultrasound if indicated.