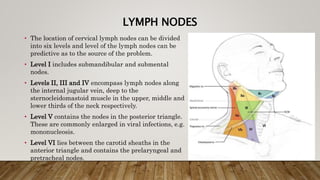
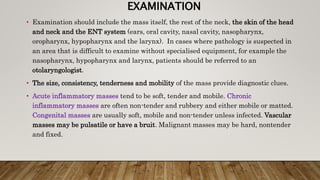
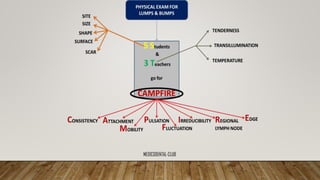
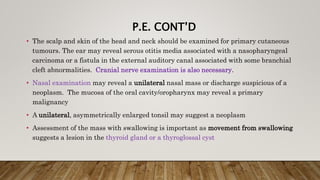
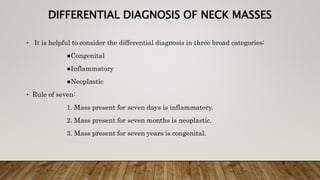
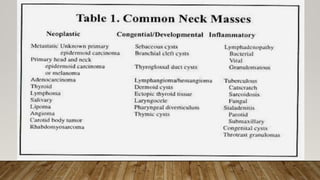
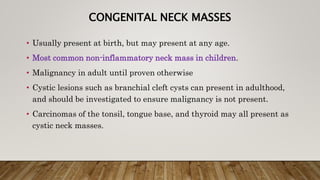
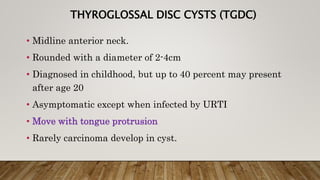
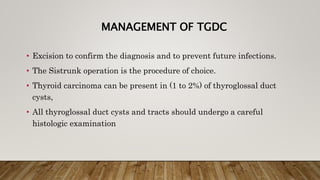
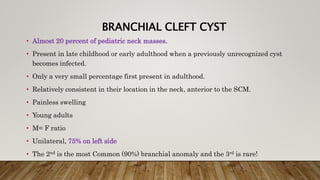
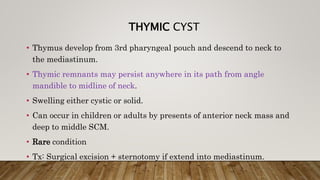
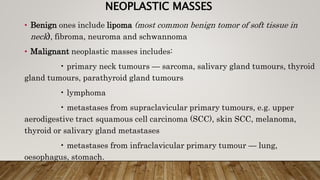
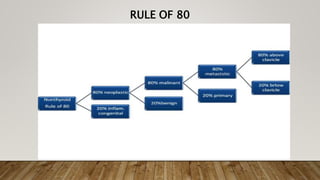
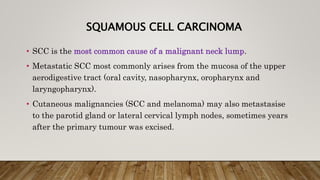
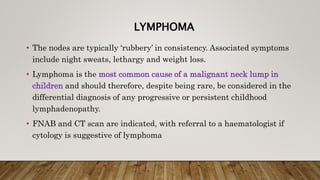
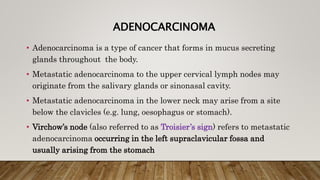
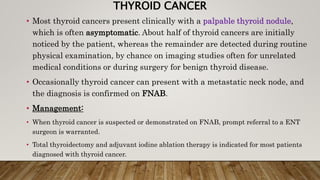
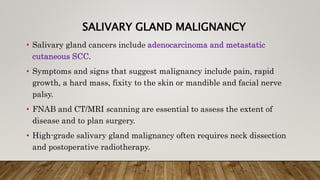
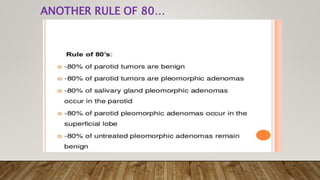
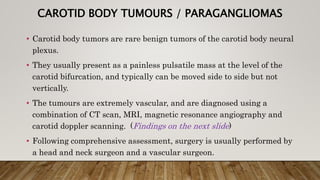
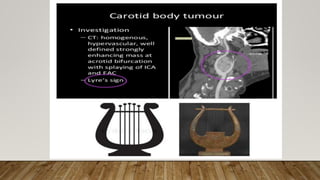
This document provides information about neck masses, including the major structures in the neck, lymph nodes, and the differential diagnosis. It discusses the major structures that can be palpated in the neck, such as the thyroid gland and lymph nodes. The differential diagnosis is divided into congenital, inflammatory, and neoplastic categories. Common congenital masses discussed include thyroglossal duct cysts, cystic hygromas, ectopic thyroid, plunging ranula, branchial cleft cyst, and dermoid cysts. Inflammatory masses are usually self-limiting.