**Overview of Neck Lumps and Surgical Anatomy**
• **Key Focus Areas**:
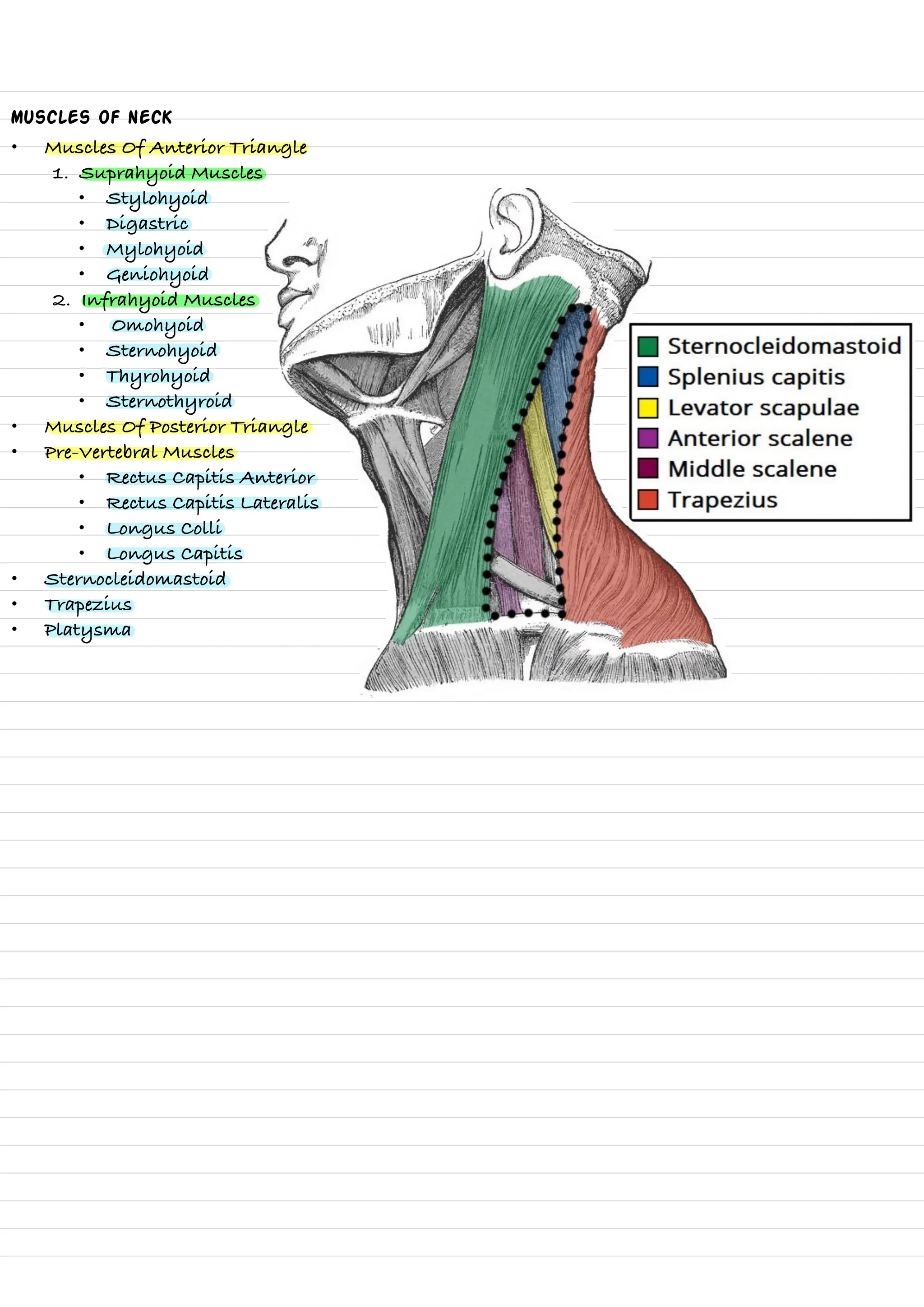
* **Surgical Anatomy of the Neck**
- Detailed breakdown of neck compartments
- Anatomical structures and layers
- Muscle groups and triangles
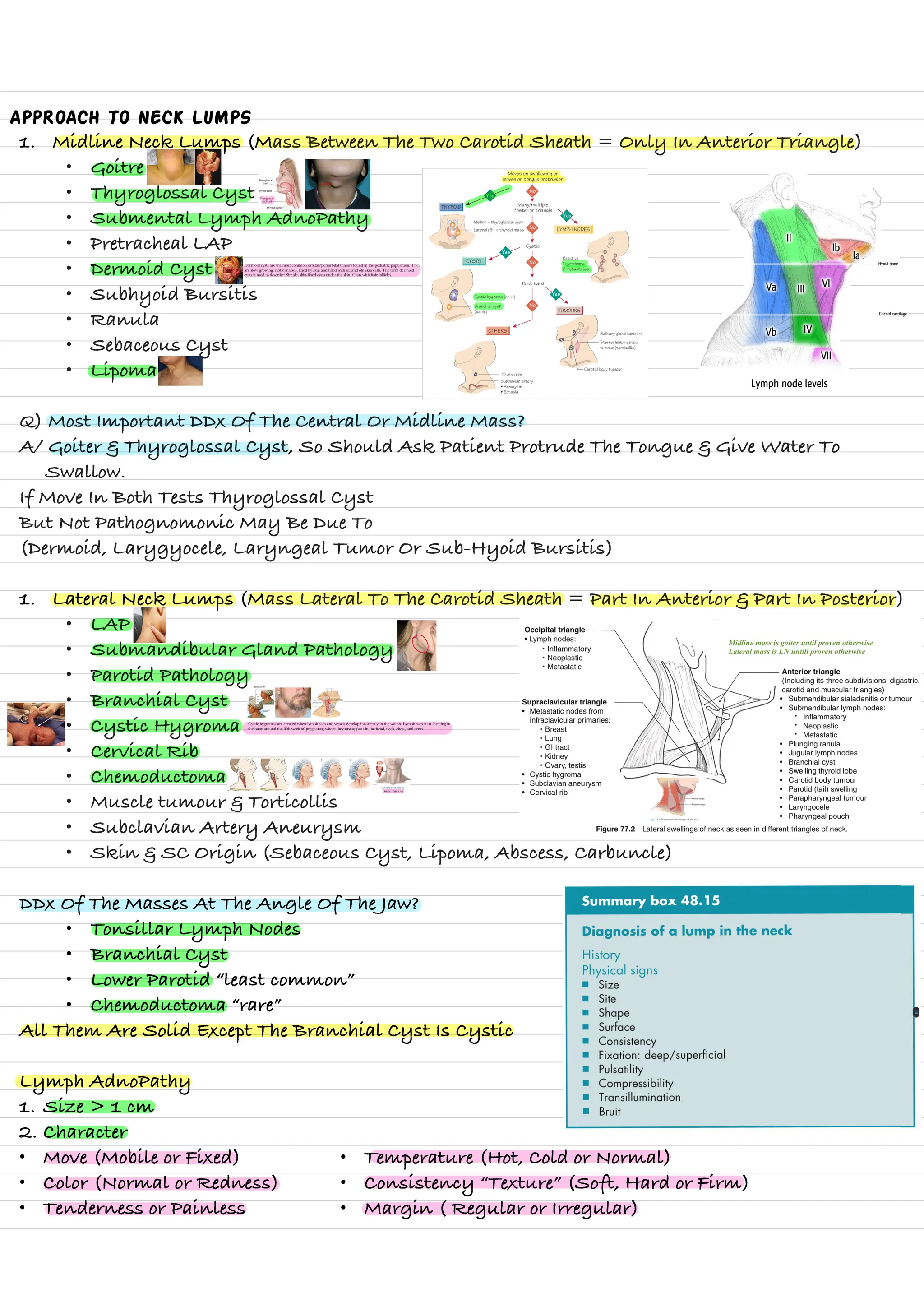
* **Neck Lump Classification**
- **Types of Neck Lumps**:
- Midline neck lumps
- Lateral neck lumps
- Congenital anomalies
- Inflammatory conditions
- Tumors
* **Diagnostic Approach**
- **Comprehensive Examination Techniques**
- Clinical assessment
- Laboratory investigations
- Imaging studies
- Biopsy methods
* **Specific Conditions Covered**
- Thyroid diseases
- Lymphadenopathy
- Cystic hygromas
- Branchial cysts
- Parathyroid disorders
• **Primary Medical Disciplines**:
* **Surgical Anatomy**
* **Endocrinology**
* **Oncology**
* **Diagnostic Medicine