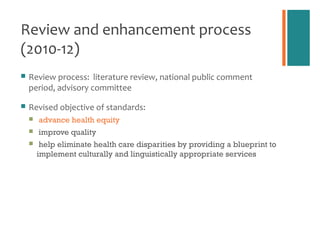
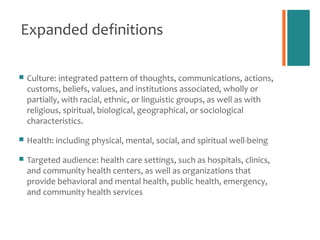
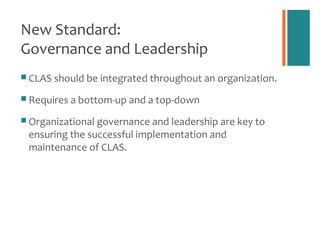
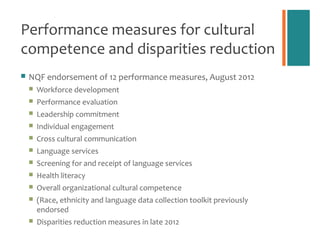
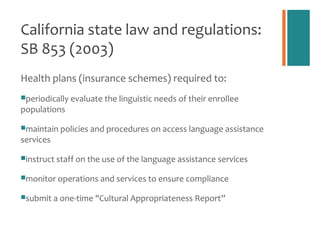
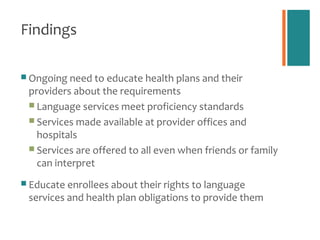
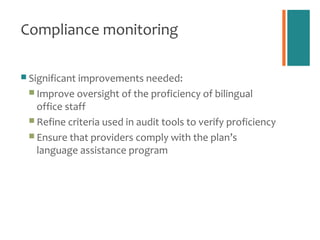
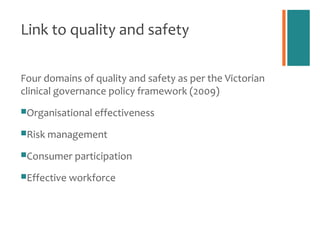
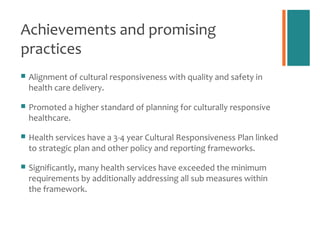
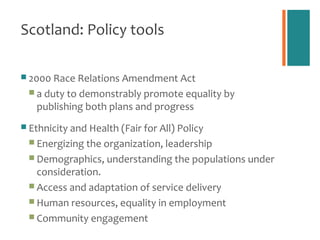
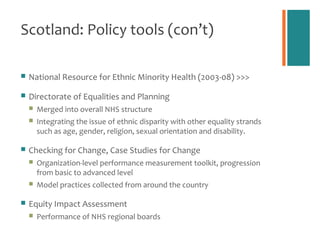
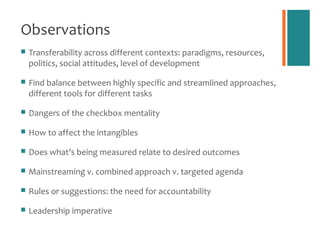
The document discusses multicultural health policy development focusing on improving culturally and linguistically appropriate services within healthcare settings. It highlights various policy tools and standards from the U.S., Australia, and Scotland aimed at promoting health equity and reducing disparities, including governance, leadership, and community engagement strategies. Key achievements, challenges, and lessons learned from implementing these policies are also addressed.