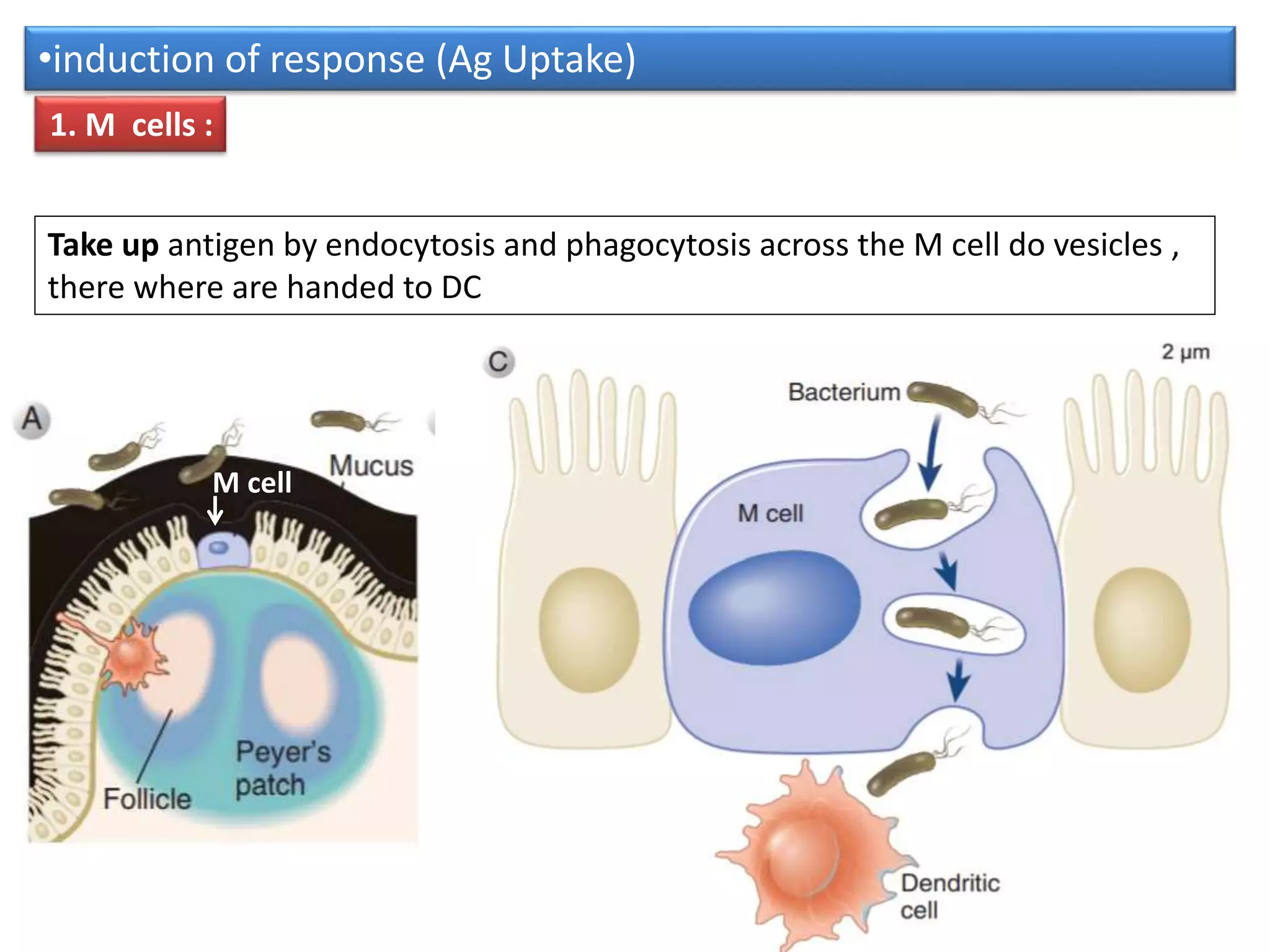
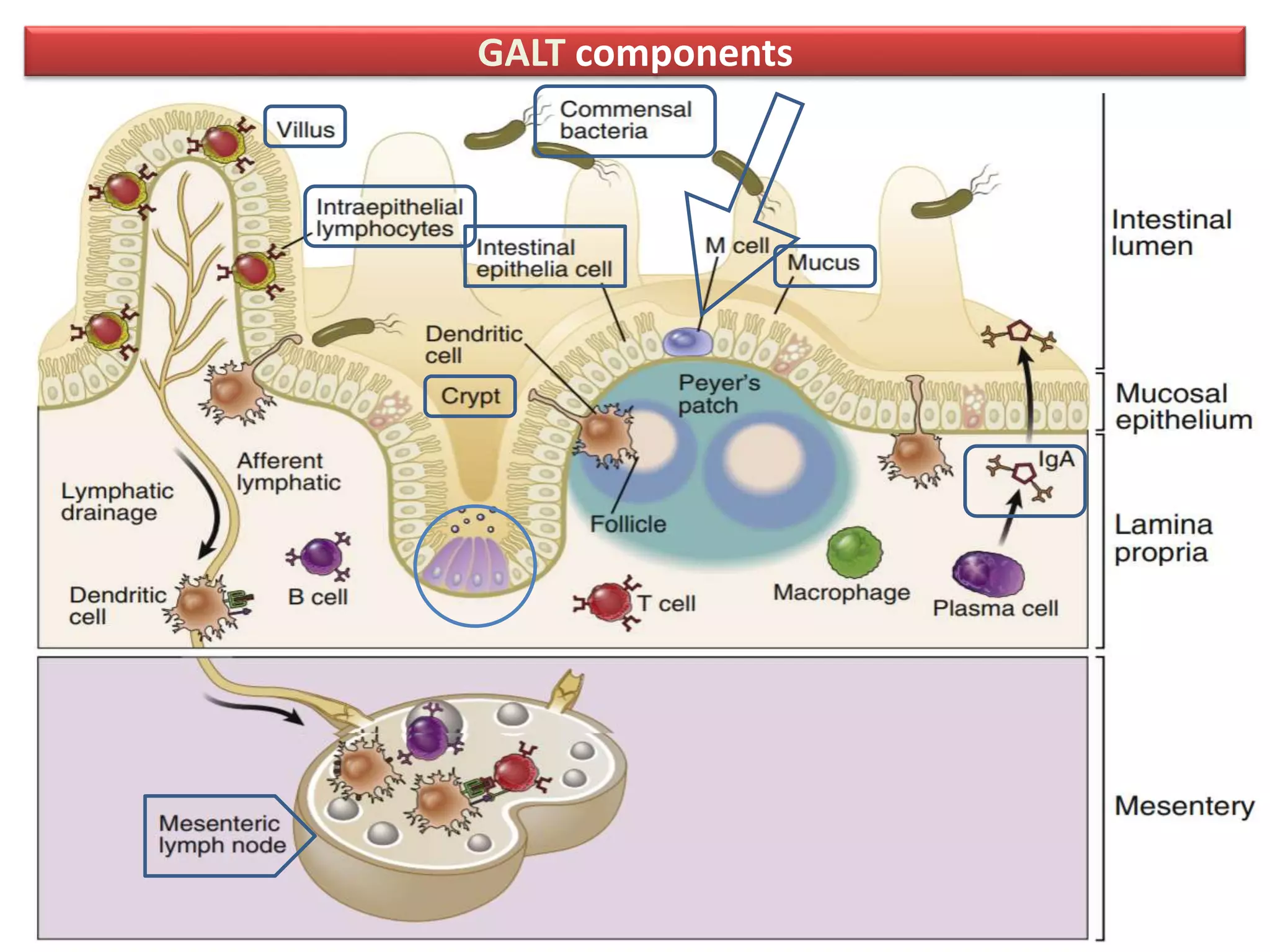
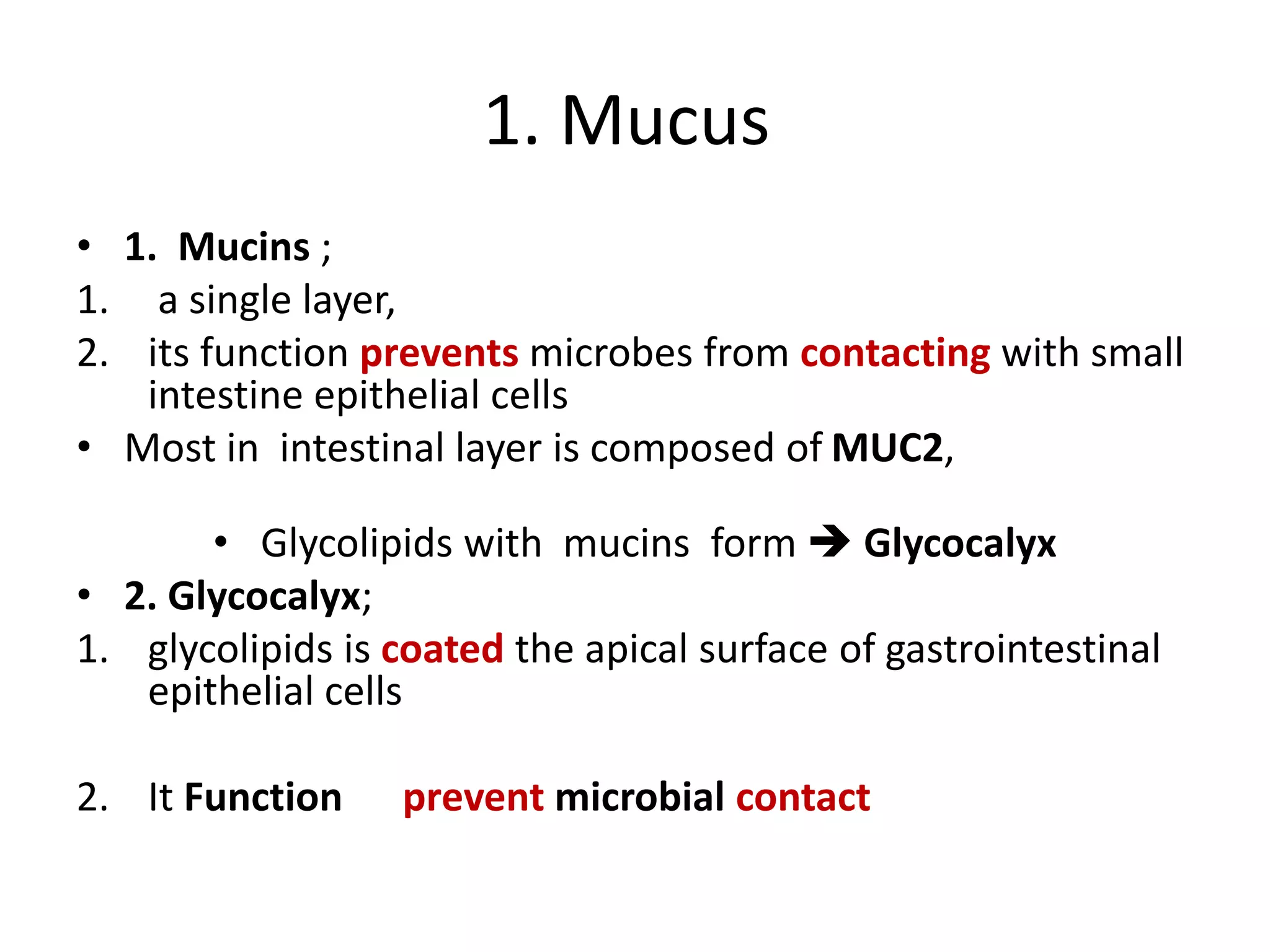
Mucosal immunity is specialized to prevent responses to harmless substances while mounting responses to pathogens. The mucosal immune system includes gut-associated lymphoid tissue (GALT) such as Peyer's patches. GALT uses innate mechanisms like mucus and defensins and adaptive responses including IgA and T cells to prevent microbial invasion while tolerating commensal bacteria. Dendritic cells sample antigens and induce regulatory or effector T cell responses depending on the antigen. Secretory IgA transported across the epithelium provides frontline protection for mucosal surfaces.






![• Increases in mucins production
• By
1. cytokines (IL-1, IL-4, IL-6, IL-9, IL-13, tumor
necrosis factor [TNF], and type I interferons)
2. neutrophil products (such as elastase),
3. and microbial adhesive proteins.](https://image.slidesharecdn.com/mucosalimmunity-230209195545-49181491/75/mucosal-immunity-pptx-10-2048.jpg)