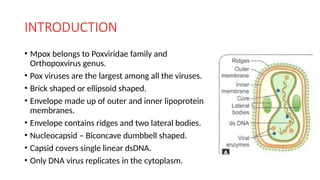
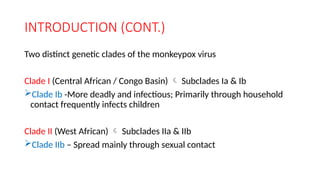
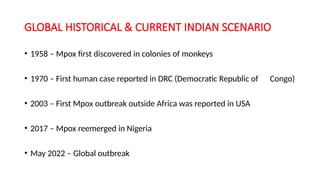
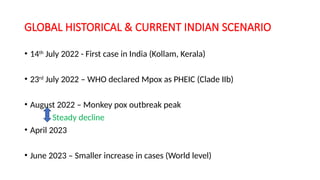
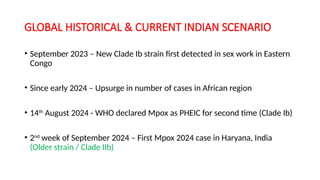
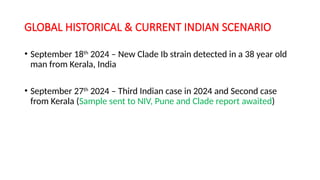
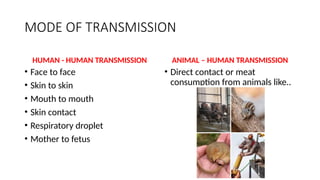
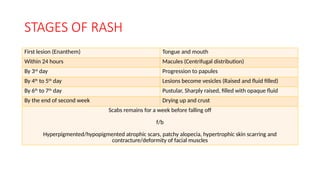
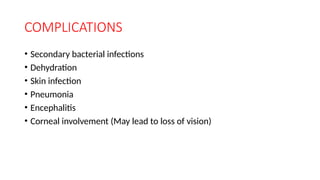
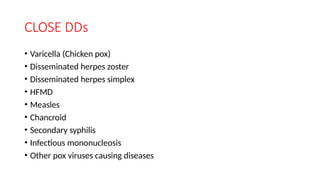
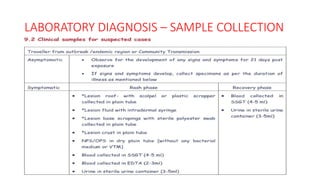
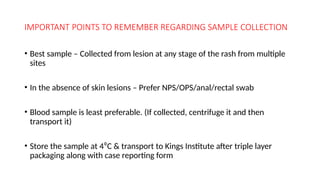
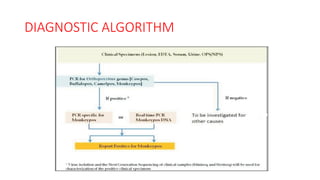
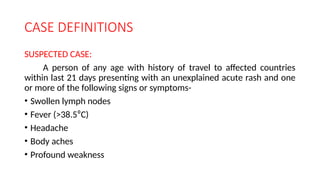
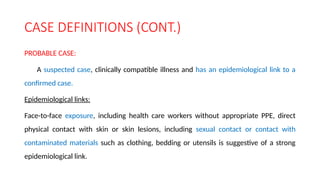
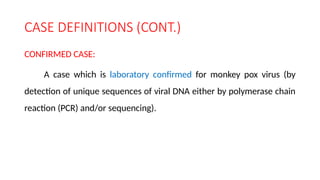
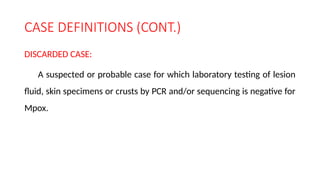
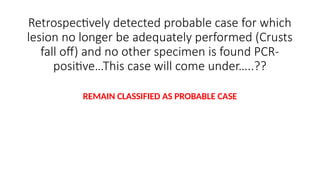
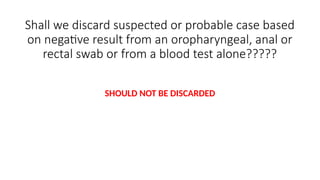
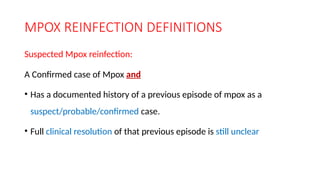
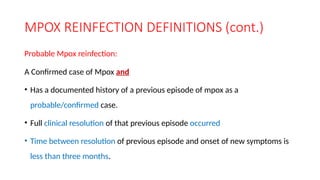
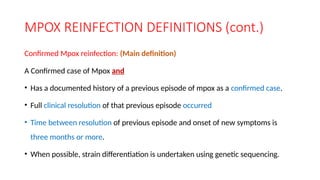
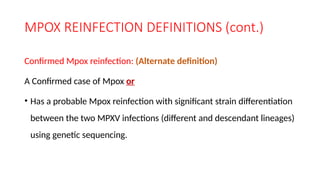
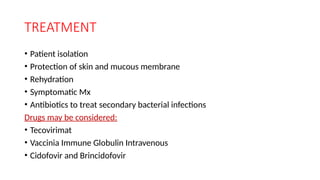
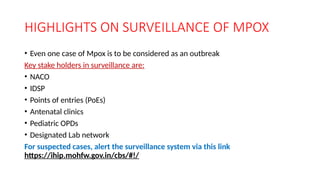
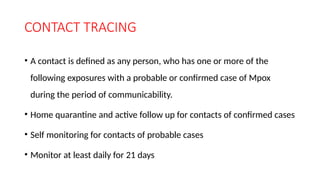
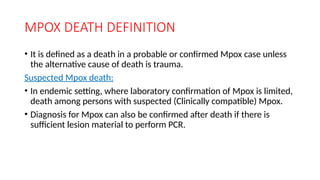
The document provides a comprehensive overview of mpox (monkeypox), detailing its classification, historical context, epidemiology, clinical features, treatment, and prevention strategies. It highlights the global and Indian scenarios, including the timeline of outbreaks and case definitions, and covers the importance of laboratory diagnosis and surveillance. Additionally, it outlines vaccination options and preventive measures for controlling the spread of the disease.