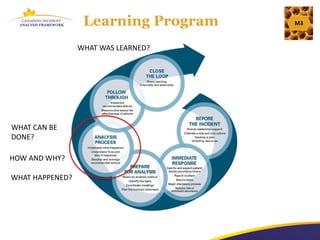
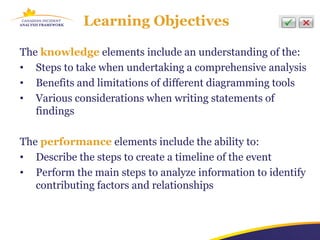
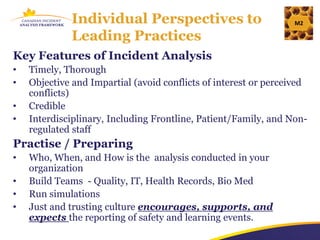
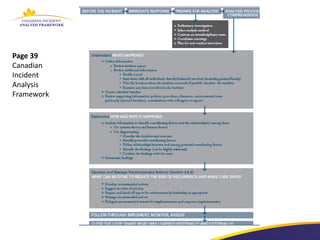
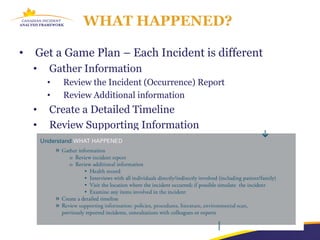
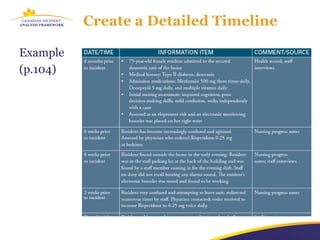
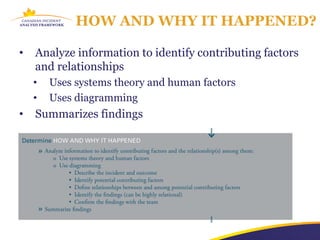
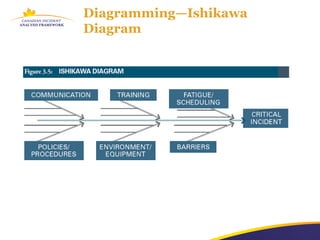
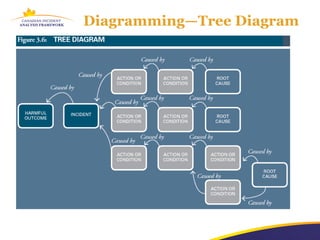
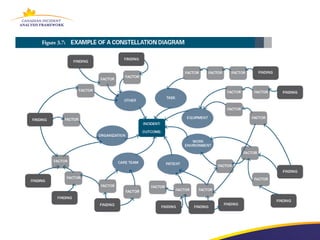
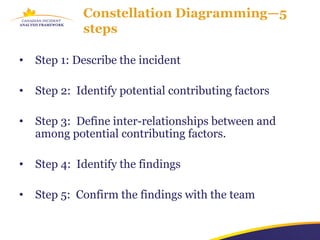
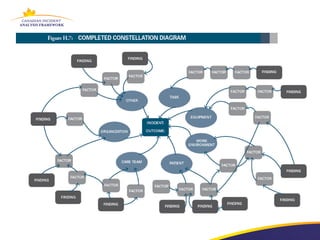
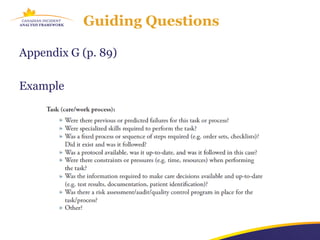
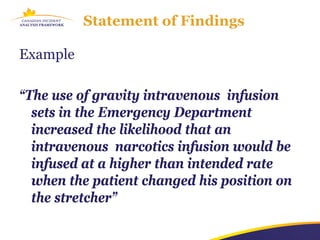
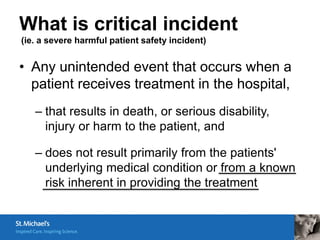
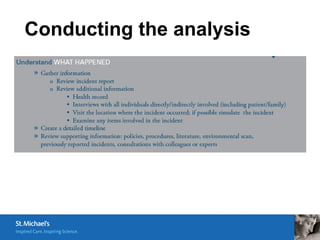
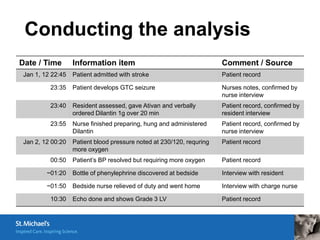
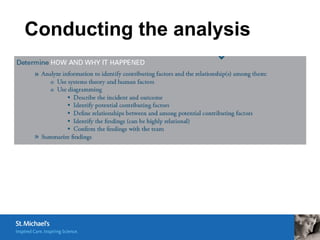
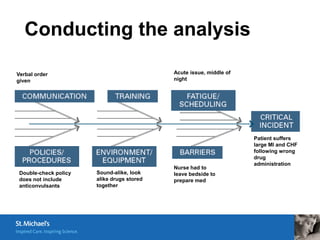
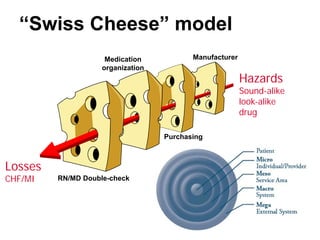
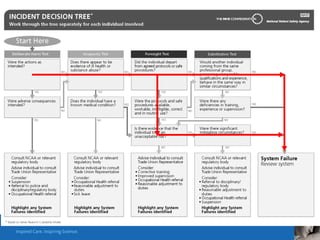
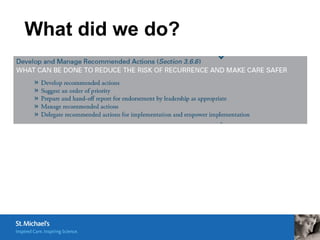
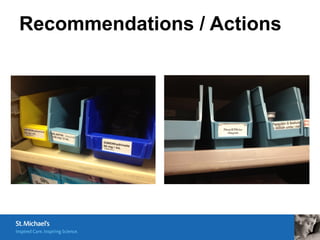
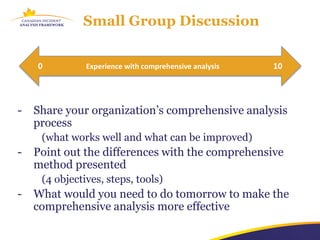
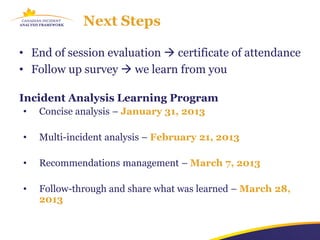
The document outlines a comprehensive incident analysis learning program, focusing on methodologies for reviewing healthcare incidents to improve patient safety. It highlights the steps involved in conducting thorough investigations, the importance of understanding contributing factors, and using diagramming tools to analyze incidents. The training emphasizes an interdisciplinary approach and effective communication to foster a culture of safety and learning in healthcare settings.