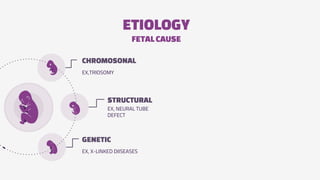
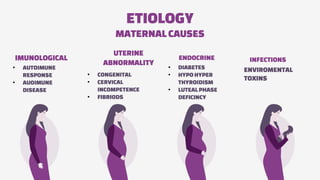
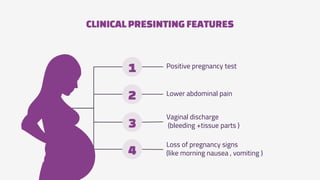
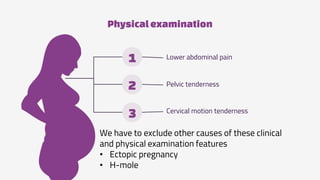
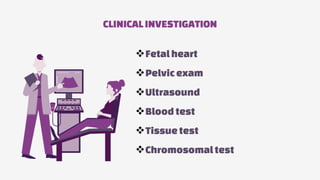
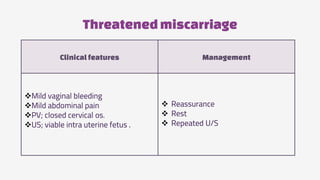
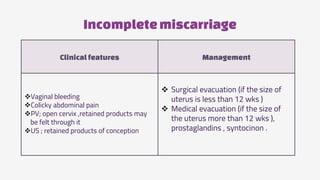
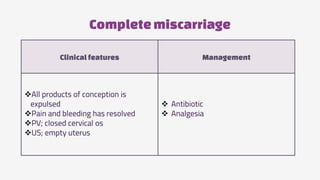
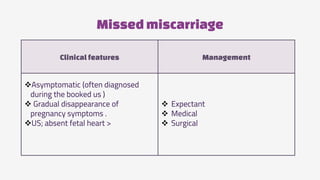
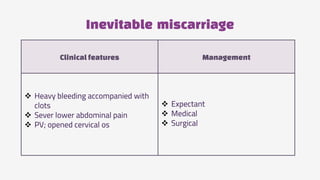
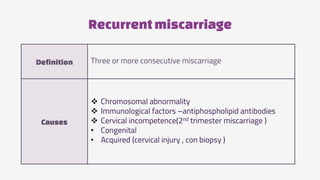
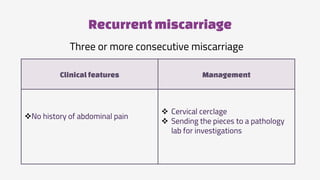
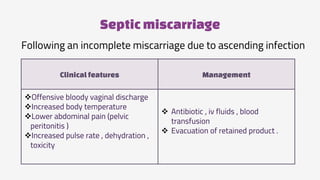
The document provides an overview of miscarriage, defining it as a spontaneous loss of pregnancy before the 24th week of gestation, with key statistics indicating that around 20% of pregnancies end in this way. It discusses various risk factors, types of miscarriage, clinical features, management strategies, and possible complications, as well as the significance of psychological impacts on affected individuals. Clinical investigations and physical examinations are emphasized for accurate diagnosis and appropriate treatment plans.