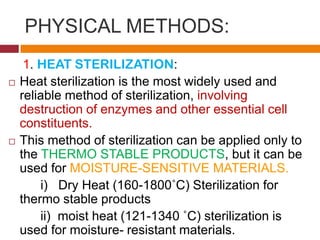
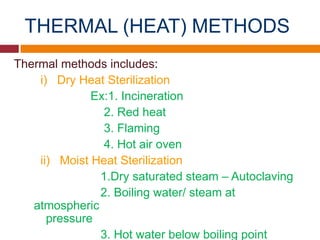
Sterilization is any process that eliminates transmissible agents like bacteria and viruses. There are physical and chemical methods of sterilization. Physical methods include heat sterilization like autoclaving, which is most widely used, as well as radiation and filtration. Heat sterilization destroys cell constituents but can only be used on thermo-stable products. Radiation sterilization uses gamma rays or electrons on dry products. Filtration removes microbes from liquids and gases. Chemical sterilization uses ethylene oxide or formaldehyde gases, which are mutagenic. Different sterilization methods have various merits and applications in pharmaceuticals and medicine.