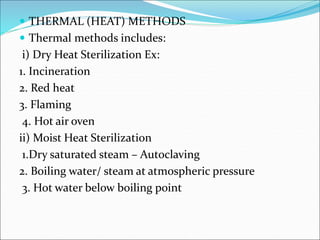
This document discusses various sterilization methods including physical (heat, radiation, filtration), chemical (gaseous), and their mechanisms and applications. Heat sterilization is the most widely used method and can be dry heat or moist heat. Radiation uses gamma rays or electrons to damage DNA. Filtration removes microbes physically. Gaseous methods like ethylene oxide act as alkylating agents. Selection depends on material properties and desired sterility level. In-process controls monitor manufacturing to ensure quality. Membrane filtration and direct inoculation are used in sterility testing.