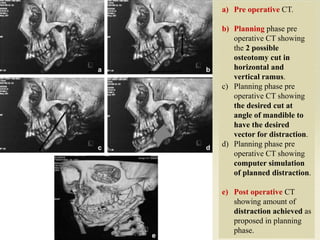
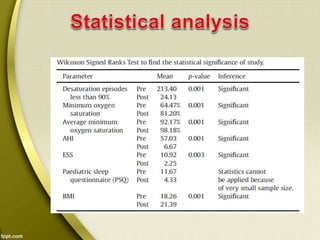
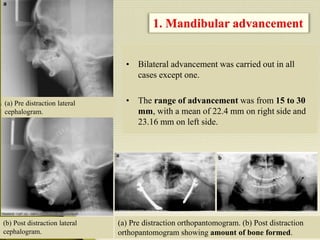
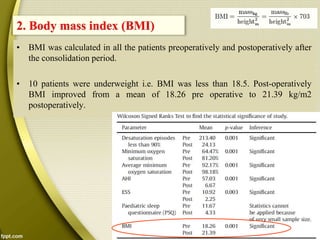
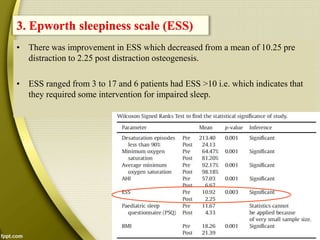
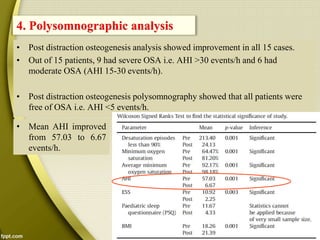
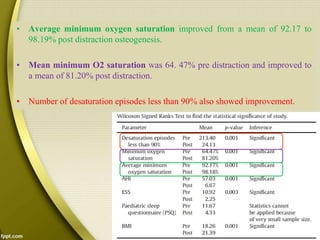
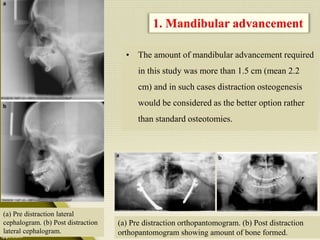
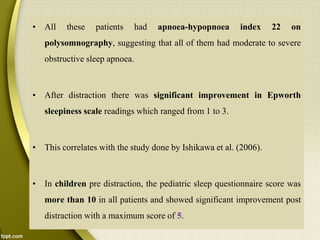
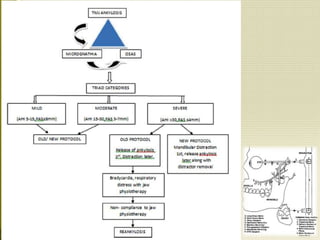
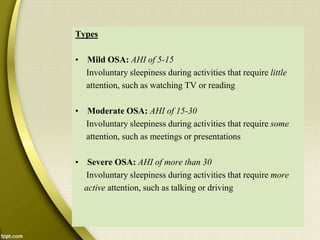
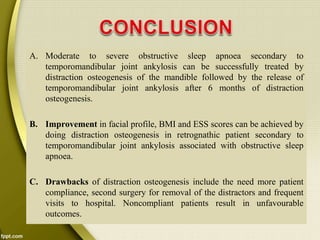
Distraction osteogenesis was performed on 15 patients with retrognathia and obstructive sleep apnea secondary to temporomandibular joint ankylosis. This study evaluated the effects of mandibular advancement using distraction osteogenesis to increase the posterior airway space. Results found significant improvements in sleep apnea symptoms and polysomnography outcomes after distraction, including reduced apnea-hypopnea index and increased lowest blood oxygen saturation. The authors concluded that distraction osteogenesis is an effective treatment for obstructive sleep apnea in patients with severe acquired retrognathia.