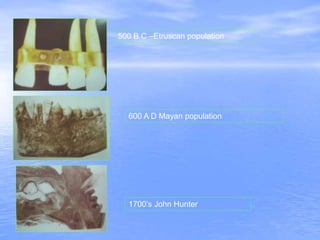
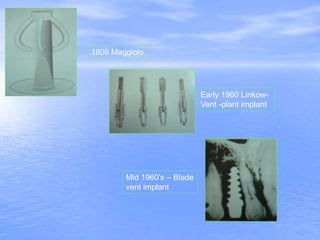
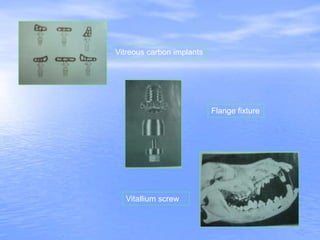
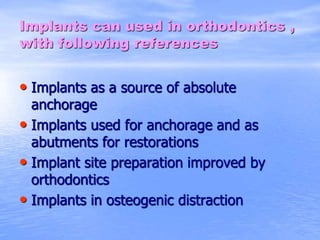
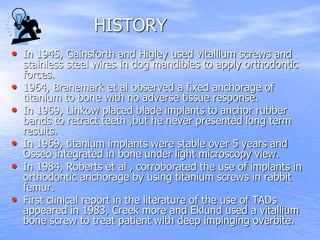
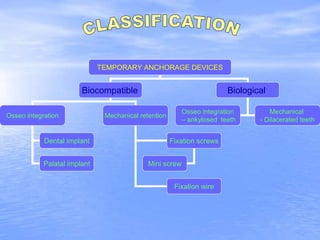
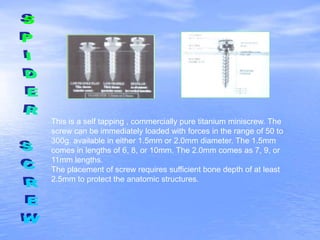
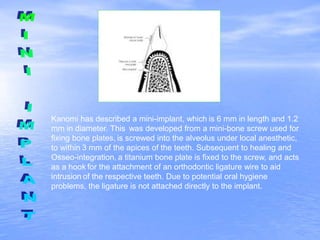
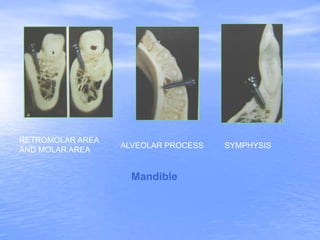
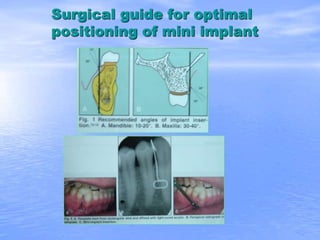
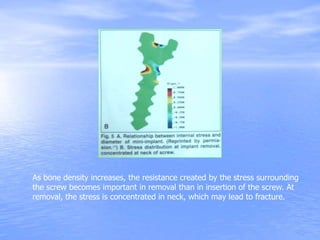
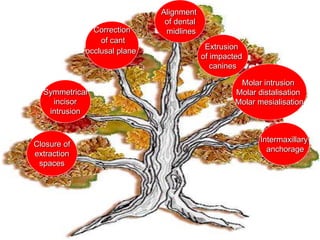
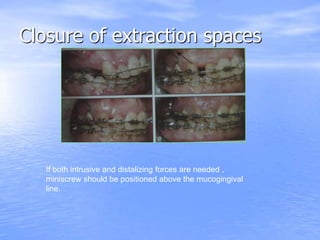
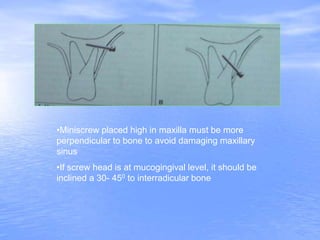
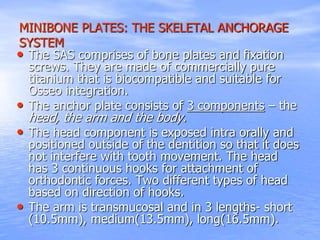
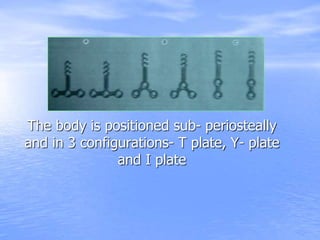
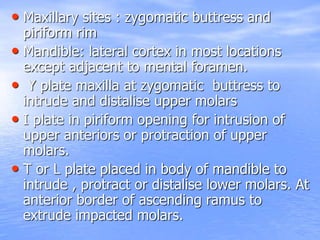
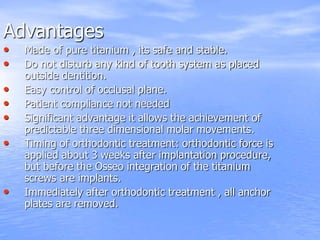
This document provides an overview of using dental implants for orthodontic anchorage. It discusses the history of implants, defines relevant terminology, and classifies implants based on position, material, size, and shape. The benefits of implants as anchorage devices and various implant designs are described. Acceptable placement sites are outlined as well as surgical procedures and bone-implant interface. Loading protocols, problems encountered, and other applications are summarized. The document concludes by referencing additional sources.