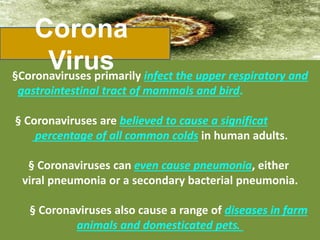
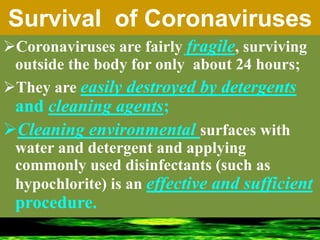
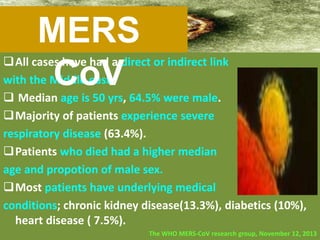
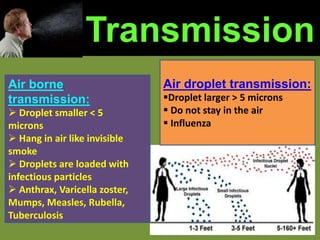
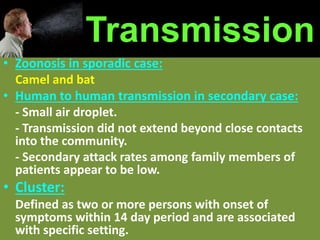
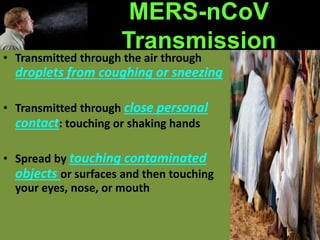
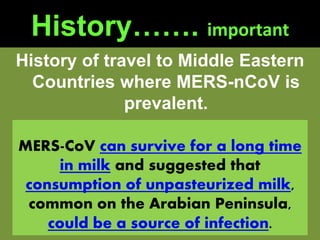
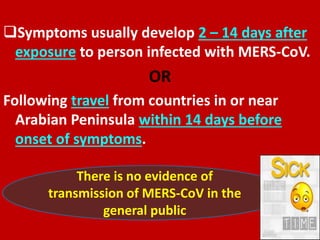
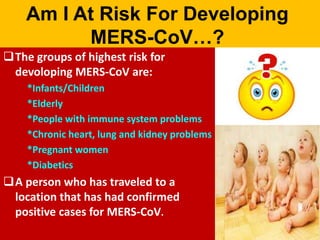
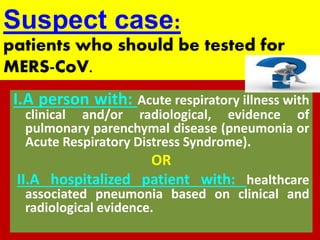
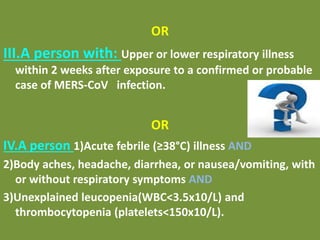
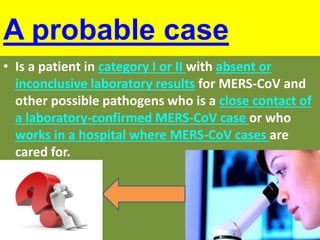
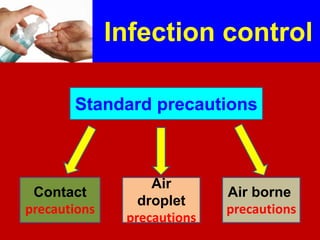
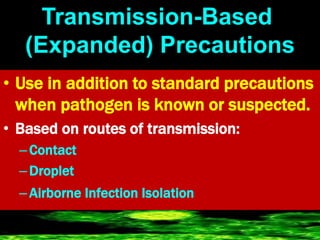
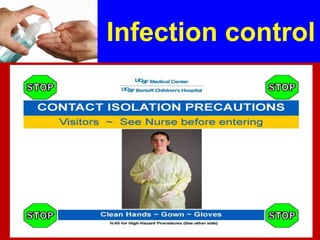
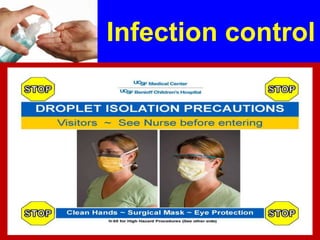
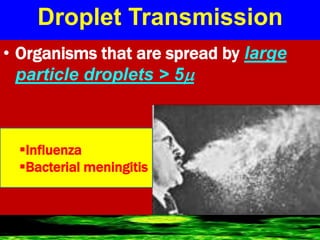
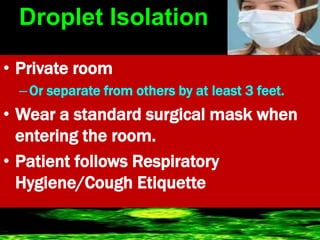
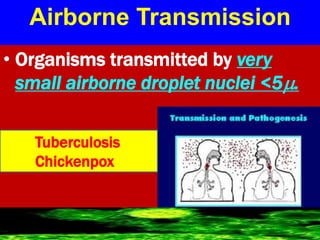
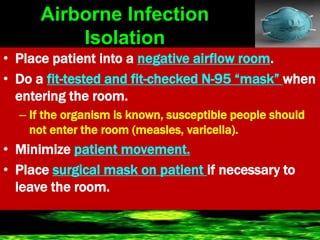
Coronaviruses can cause respiratory illnesses in humans ranging from the common cold to more severe diseases like MERS and SARS. They are transmitted through airborne droplets and contaminated surfaces. While most coronavirus infections cause mild illness, MERS can lead to severe pneumonia and organ failure. At risk groups include the elderly, immunocompromised, and those with chronic conditions. Treatment focuses on supportive care, while prevention emphasizes hand hygiene, respiratory etiquette, and personal protective equipment for healthcare workers.