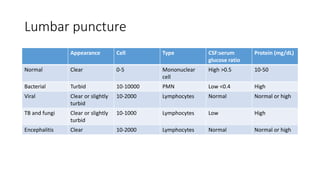
Meningitis is an inflammation of the meninges, the protective membranes surrounding the brain and spinal cord. It commonly affects children under 4 years old. The etiology depends on age, with common causes in neonates being GBS, E. coli, and Listeria monocytogenes. Symptoms include fever, vomiting, irritability, and neck stiffness. Diagnosis involves lumbar puncture to examine CSF for elevated white blood cells. Treatment involves supportive care and antibiotics targeting the suspected pathogen. Prevention strategies include vaccination against common causes like meningococcus and Hib.