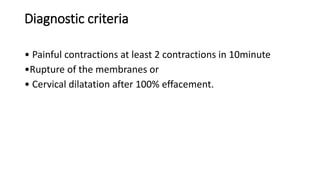
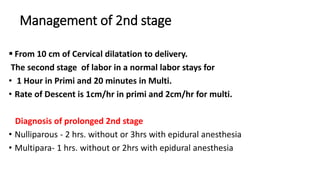
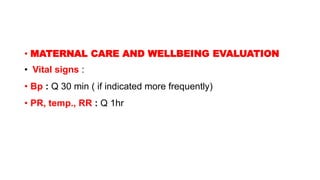
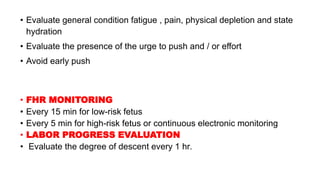
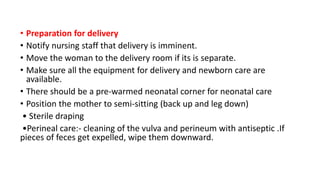
This document outlines the management of the three stages of labor. The first stage involves monitoring the mother's vital signs and positioning, providing nutrition and pain management, as well as fetal heart rate monitoring and assessing cervical dilation. The second stage focuses on monitoring the mother's vitals and pushing efforts, as well as fetal descent. Procedures like episiotomy and delivery of the baby are also described. The third stage involves active management with uterotonic drugs, controlled cord traction, and uterine massage to achieve a quick delivery and reduce bleeding.