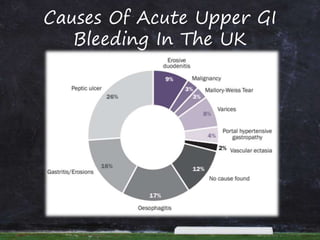
- Acute upper gastrointestinal bleeding is a common medical emergency that can have high mortality.
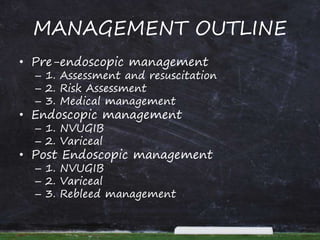
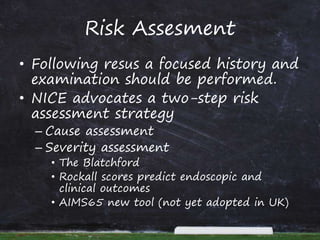
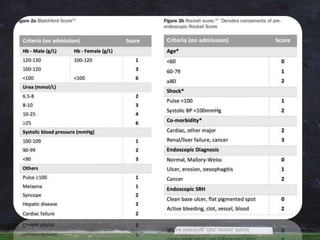
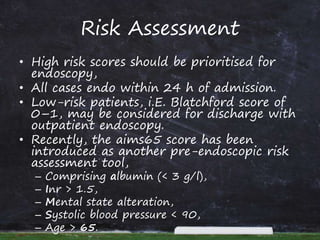
- Risk assessment using tools like the Blatchford and Rockall scores helps determine urgency of endoscopy and predict outcomes.
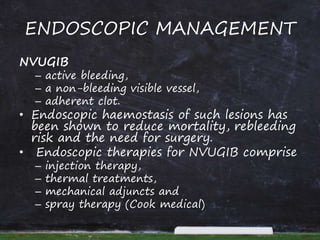
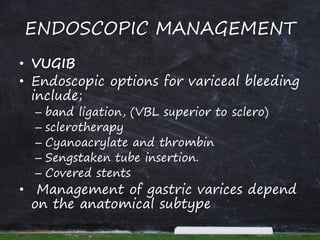
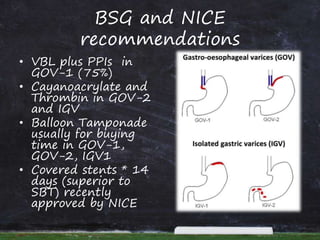
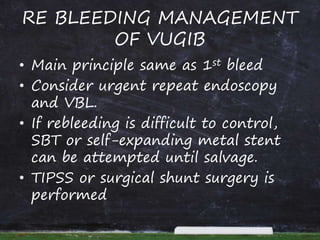
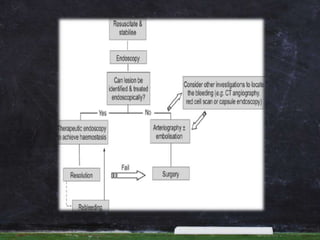
- Endoscopy within 24 hours of admission is recommended to treat bleeding lesions through methods like injection, thermal coagulation, or band ligation of varices.
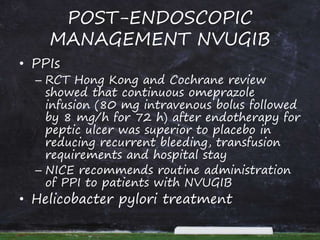
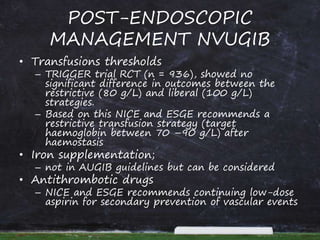
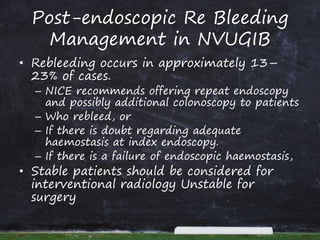
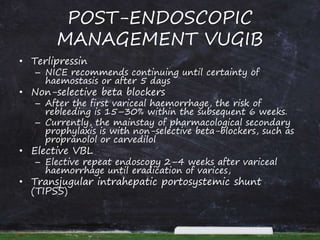
- Post-endoscopic management involves PPIs, transfusions targeting a hemoglobin of 70-90 g/L, H. pylori treatment if present, and continued medications like terlipressin or beta blockers to prevent rebleeding.