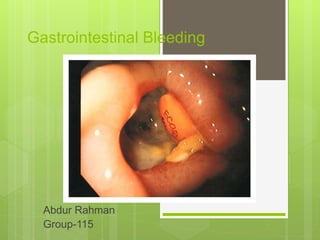
This document discusses the management of gastrointestinal bleeding. It covers the clinical presentation and definitions of acute upper and lower GI bleeding. The core principles of GI bleeding management are outlined as assessing and stabilizing hemodynamic status, determining the source of bleeding, stopping active bleeding, treating any underlying abnormalities, and preventing recurrent bleeding. Specific causes, diagnostic evaluations, endoscopic and surgical treatments are described for various types of acute GI bleeding.