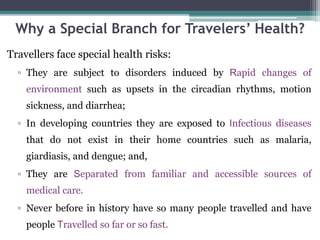
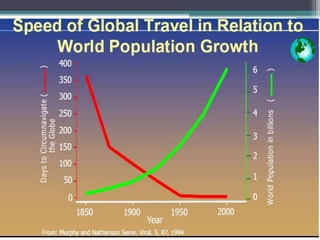
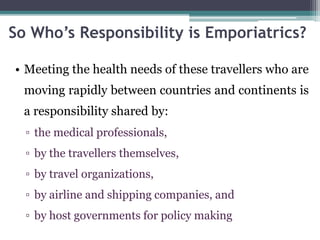
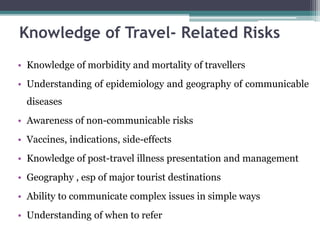
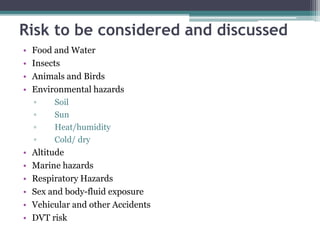
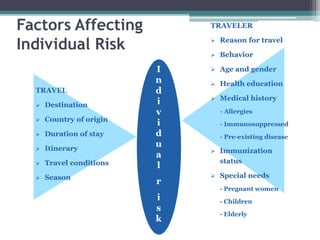
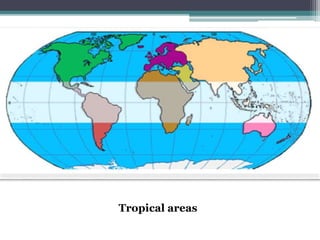
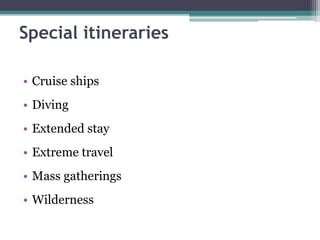
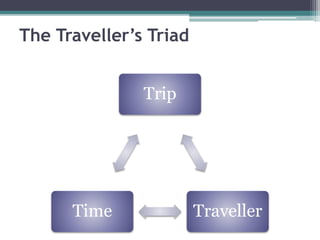
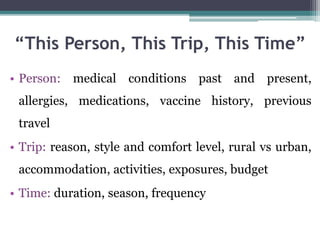
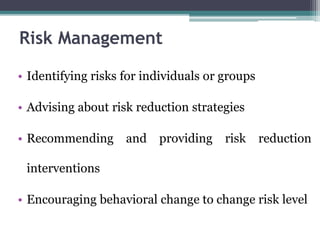
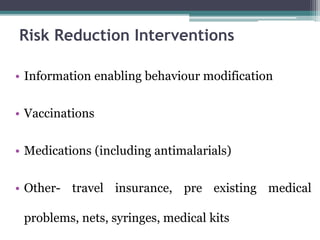
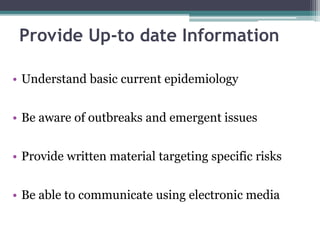
Emporiatrics is the science of promoting and protecting the health of international travelers. It is a fast-growing specialty due to the rise in international travel. Emporiatrics aims to advise travelers on health risks specific to their itinerary and reduce risks through prevention interventions like vaccines, medications, and health education. Providing individualized travel health consultations and recommendations tailored to the traveler's needs, trip details, and timeline is important for effective risk management.