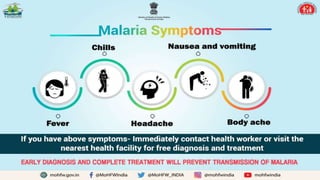
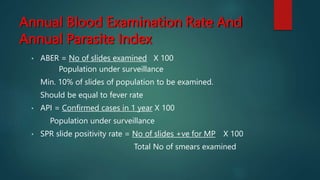
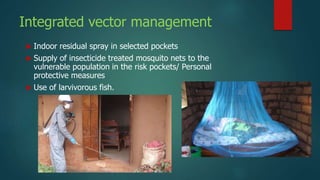
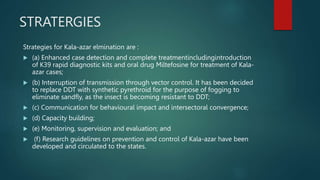
The National Vector Borne Disease Control Program (NVBDCP) focuses on the prevention and control of diseases like malaria, dengue, chikungunya, and others through various strategies, including elimination frameworks and vector management. The document outlines specific goals for malaria elimination by 2030, along with the categorization of states based on their malaria transmission levels and corresponding interventions to control these diseases. It emphasizes the importance of surveillance, early diagnosis, and community involvement in managing vector-borne diseases.