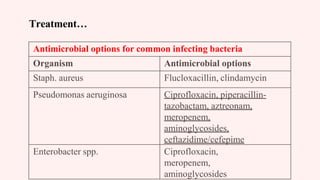
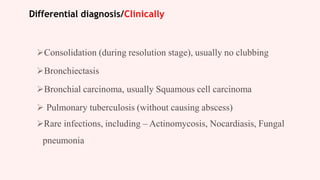
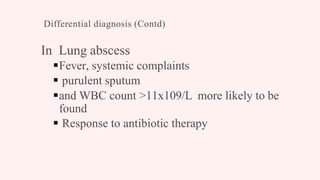
This document discusses lung abscess, including definitions, classifications, causes, risk factors, clinical manifestations, investigations, and management. It begins with defining pneumonia and classifying it based on anatomy and pathogen. Common causes of pneumonia by age group and risk factors are discussed. Clinical manifestations of pneumonia include fever, cough, chest pain, and dyspnea. The document then defines a lung abscess and classifies it as acute or chronic based on duration and etiology. Causes include aspiration, bronchial obstruction, and spread from other sites of infection. Risk factors for gram-negative colonization are listed. Symptoms of a lung abscess include cough, foul sputum, hemoptysis, and chest pain. Invest

































![Causes…
E)Haematogenous spread from a distal site [from
other infection as septic emboli]
Urinary tract infection
Abdominal sepsis
Pelvic sepsis
Infective endocarditis (right-sided)
Intravenous drug abuse
Infected IV cannulae
Septic thrombophlebitis
Salpingitis
Appendicitis
Pyaemia/ Septicaemia](https://image.slidesharecdn.com/lungabscess-230525155641-ad794246/85/LUNG-ABSCESS-pptx-40-320.jpg)