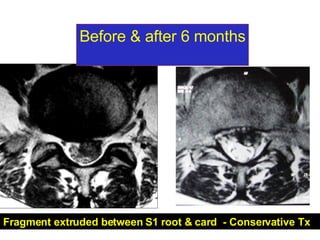
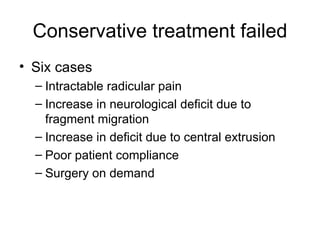
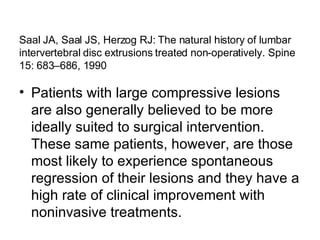
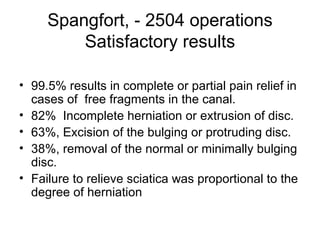
The document discusses the management of lumbar disc herniation with free fragments. It states that over 50% reduction in fragment size on follow-up MRI is clinically significant, and larger fragments have better chances of reduction and clinical outcome with conservative treatment. Conservative treatment is the initial protocol, including bed rest and avoidance of sitting and traction. Surgery may be considered if conservative treatment fails or neurological deficits increase.