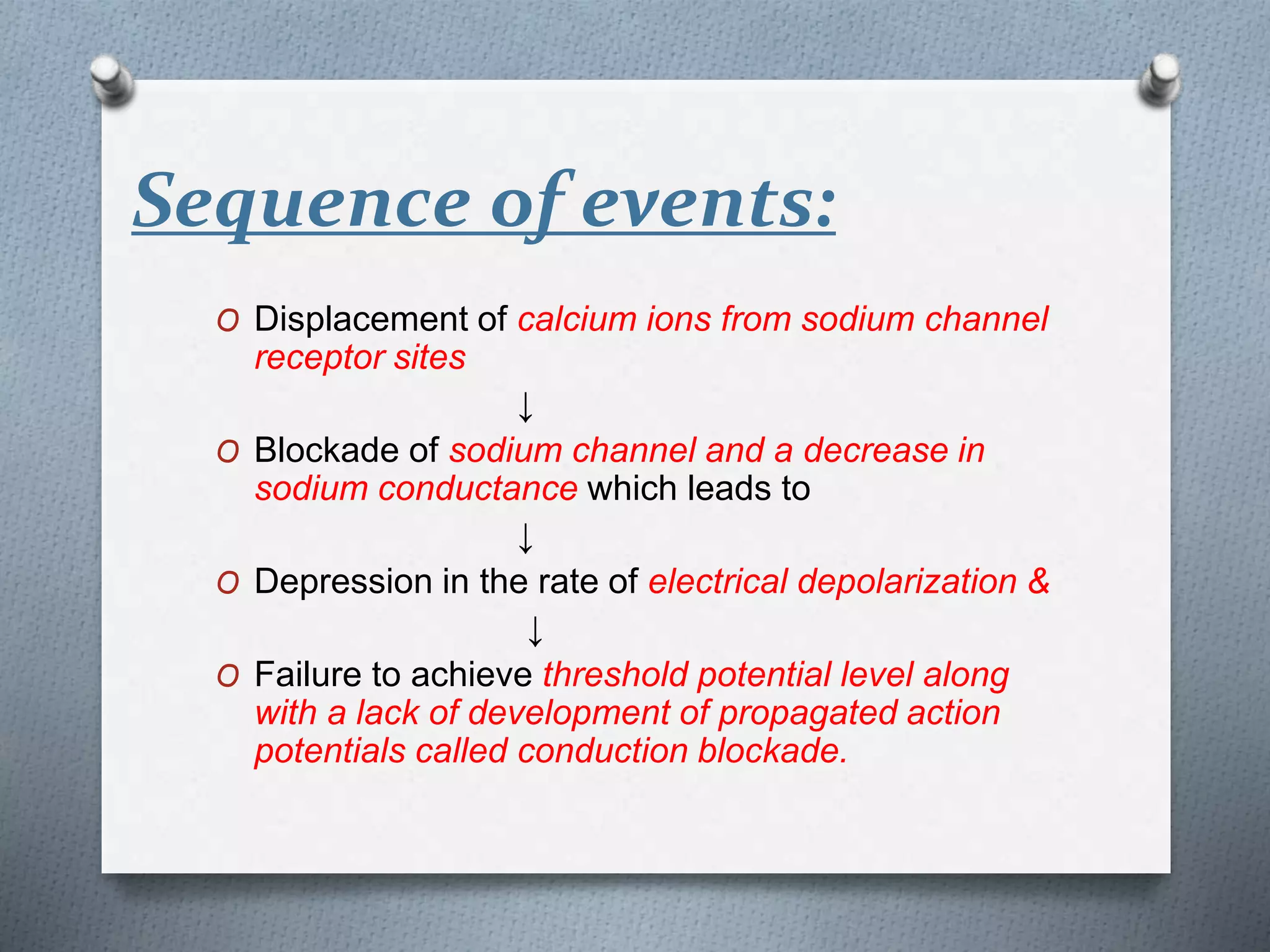
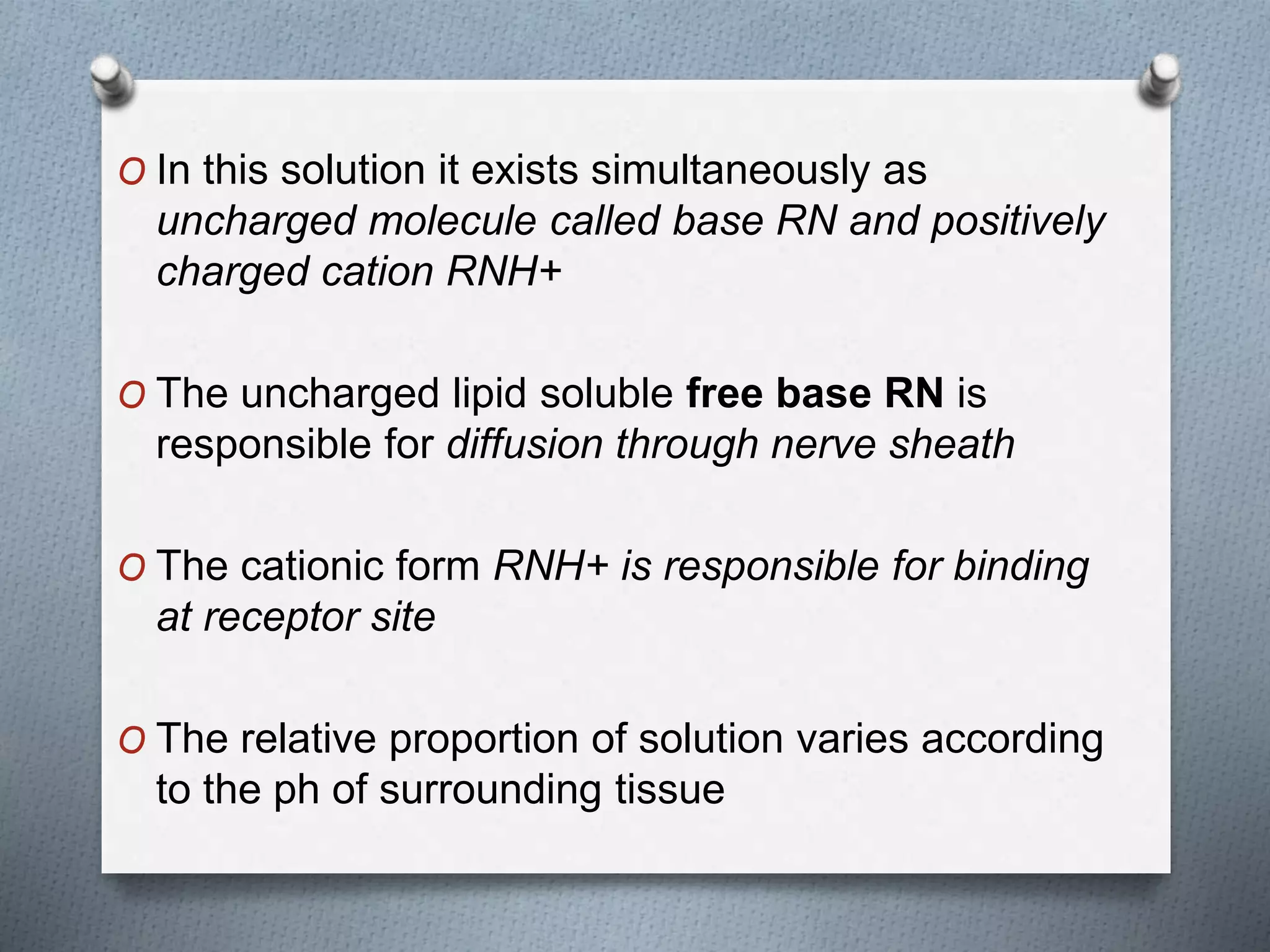
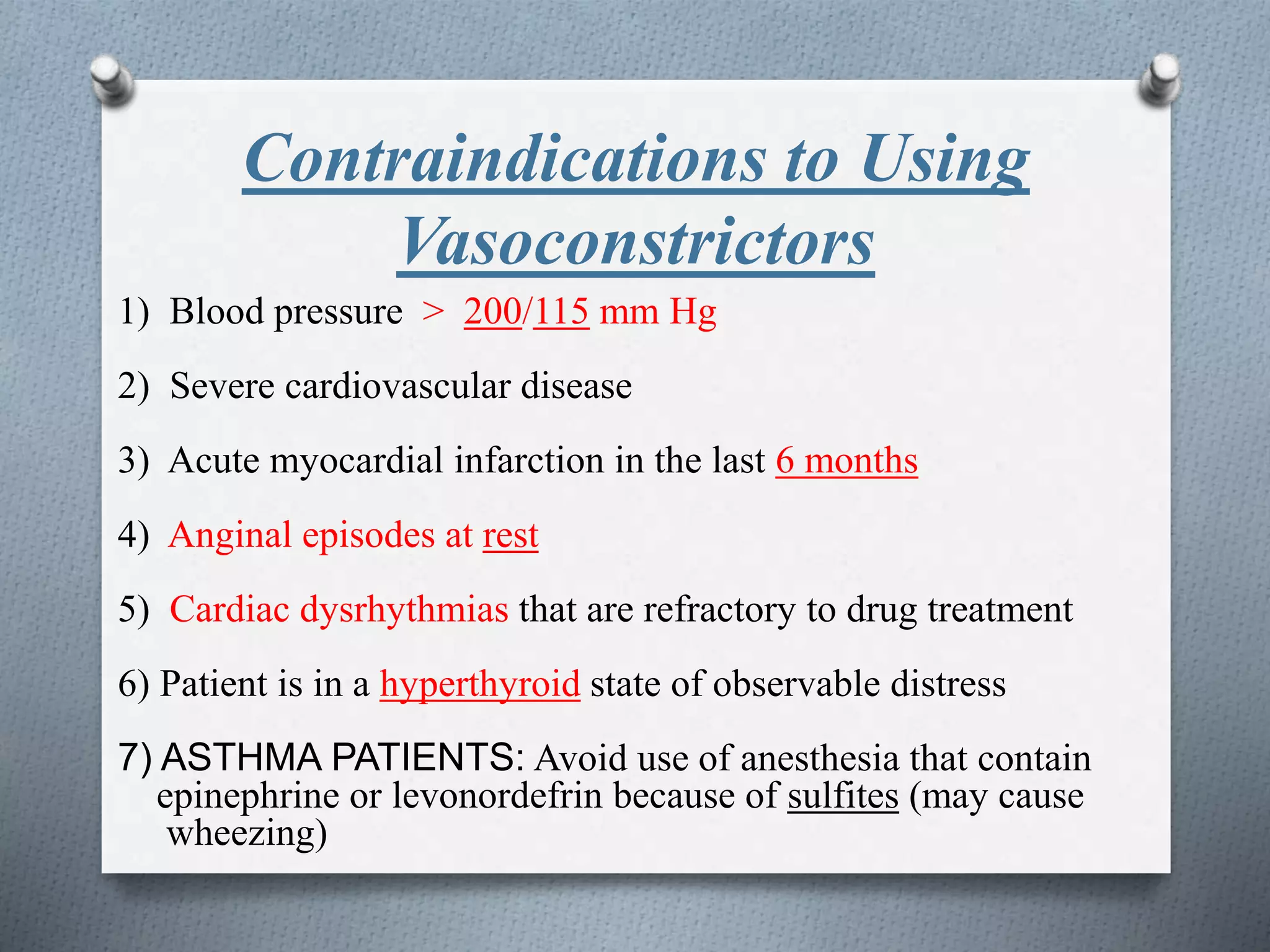
Local anesthesia produces loss of sensation in a specific area without loss of consciousness. It is commonly used in dentistry for procedures like tooth extractions, fillings, and surgery to relieve pain. Local anesthetics work by depressing nerve conduction, preventing the generation and conduction of nerve impulses. They are contraindicated in patients with certain medical conditions like infections, liver or kidney disease, or cardiac issues.