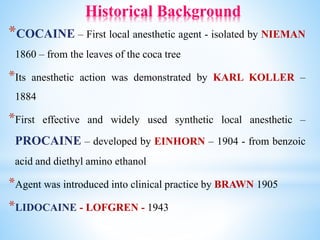
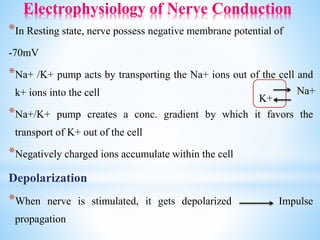
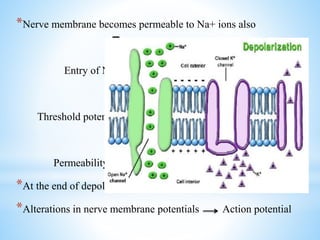
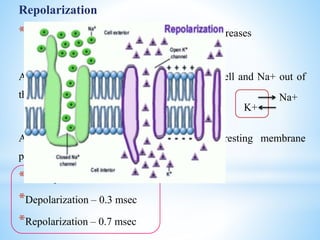
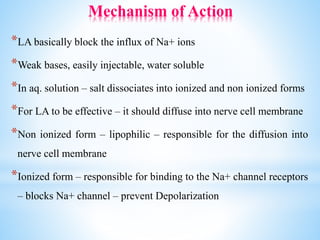
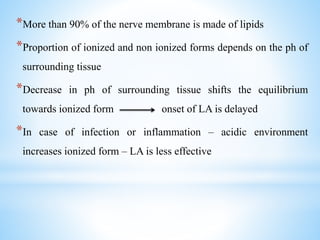
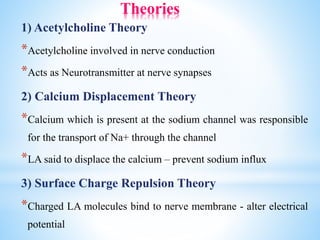
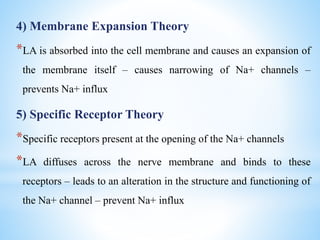
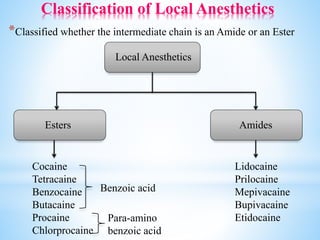
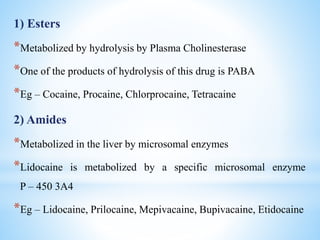
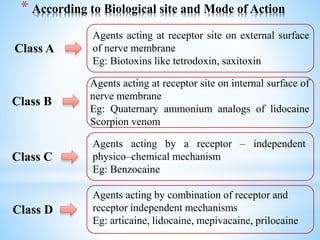
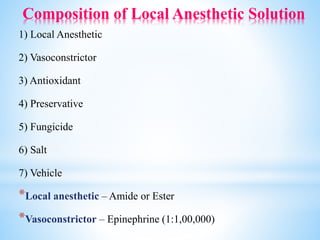
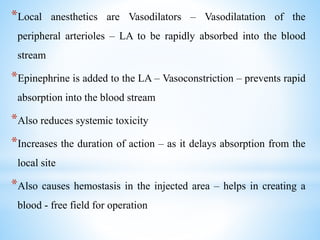
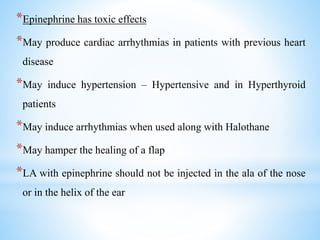
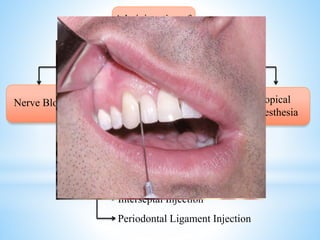
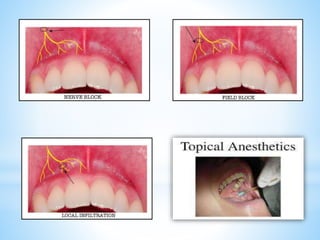
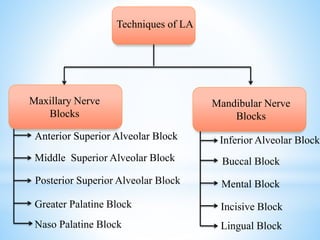
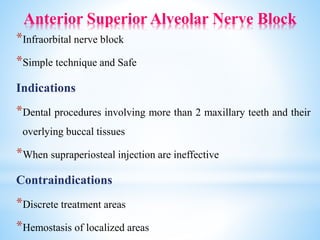
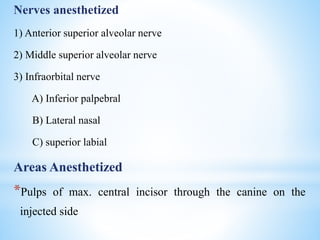
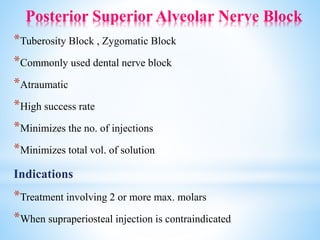
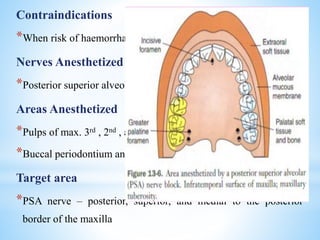
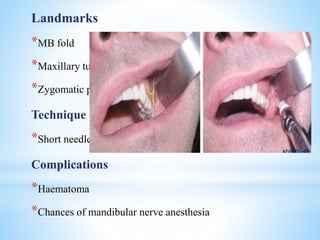
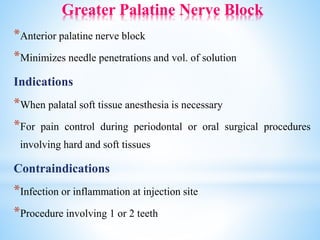
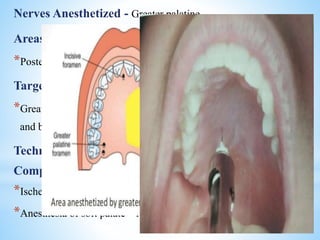
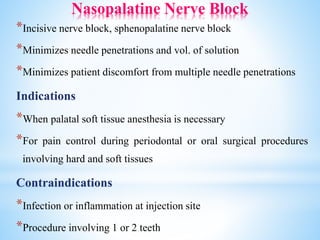
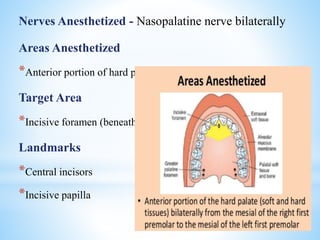
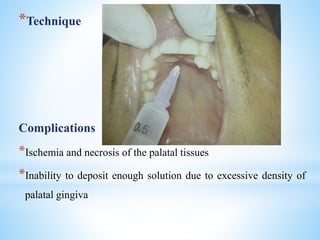
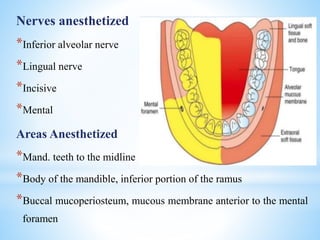
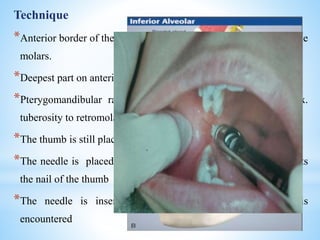
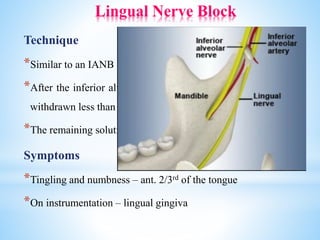
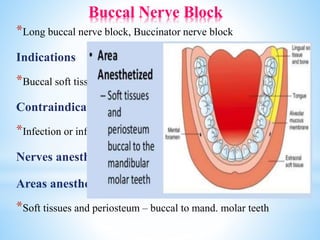
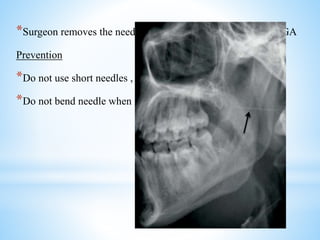
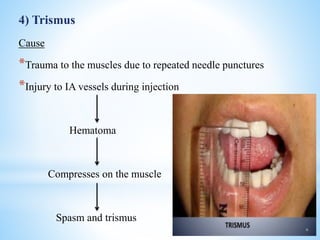
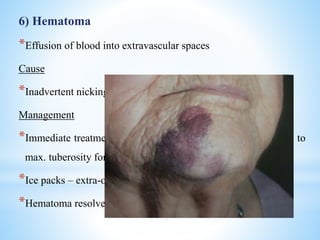
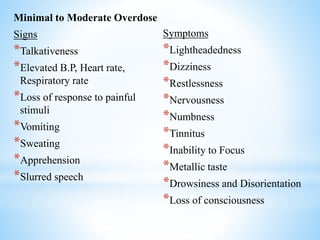
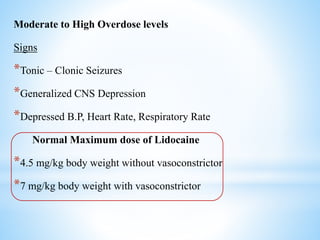
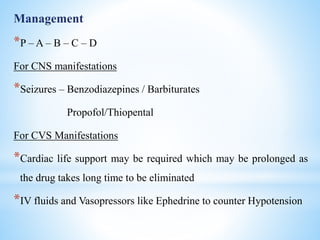
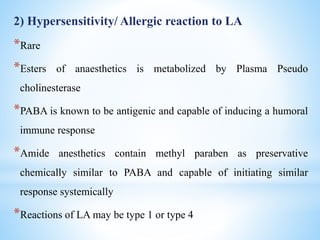
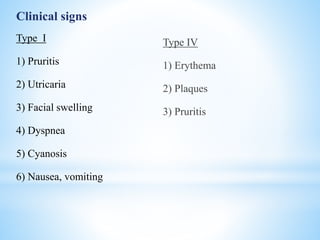
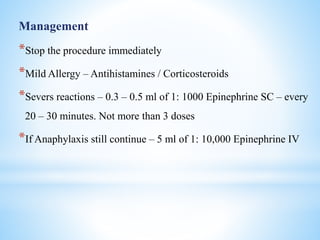
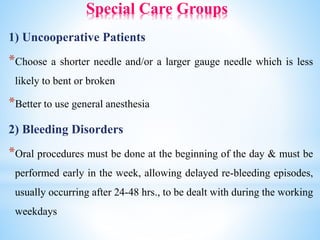
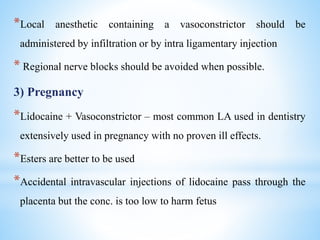
The document comprehensively outlines local anesthesia, detailing its historical background, definition, desirable properties, mechanisms of action, classifications, and various administration techniques. It describes the physiological basis of nerve conduction and the interaction of anesthetics with nerve membranes, alongside the types of local anesthetics categorized as esters or amides. Additionally, the document covers potential complications and important considerations for special care groups, ensuring a clear understanding of local anesthetic practices within medical and dental contexts.