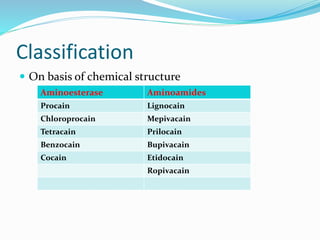
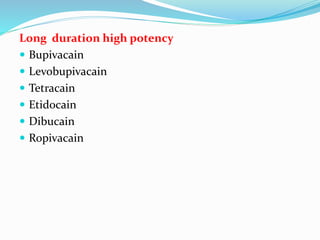
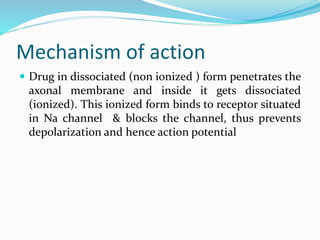
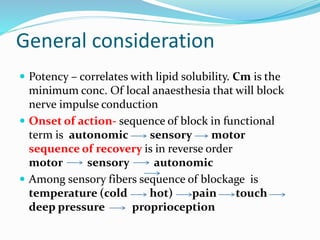
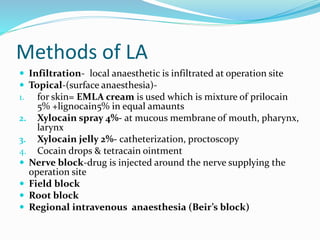
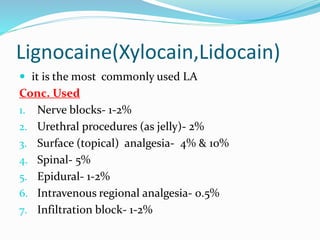
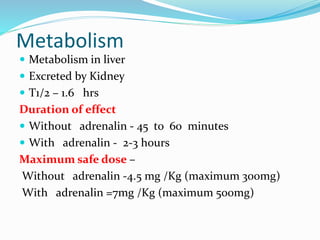
The document outlines the use of local anesthesia techniques, their advantages and disadvantages, and their classification based on chemical structure and duration of action. It describes the mechanism of action, methods of administration, and dosing guidelines for different local anesthetic agents like lidocaine and bupivacaine. Additionally, it covers other considerations like drug metabolism, safe dosing limits, and alternative uses in medical treatment.