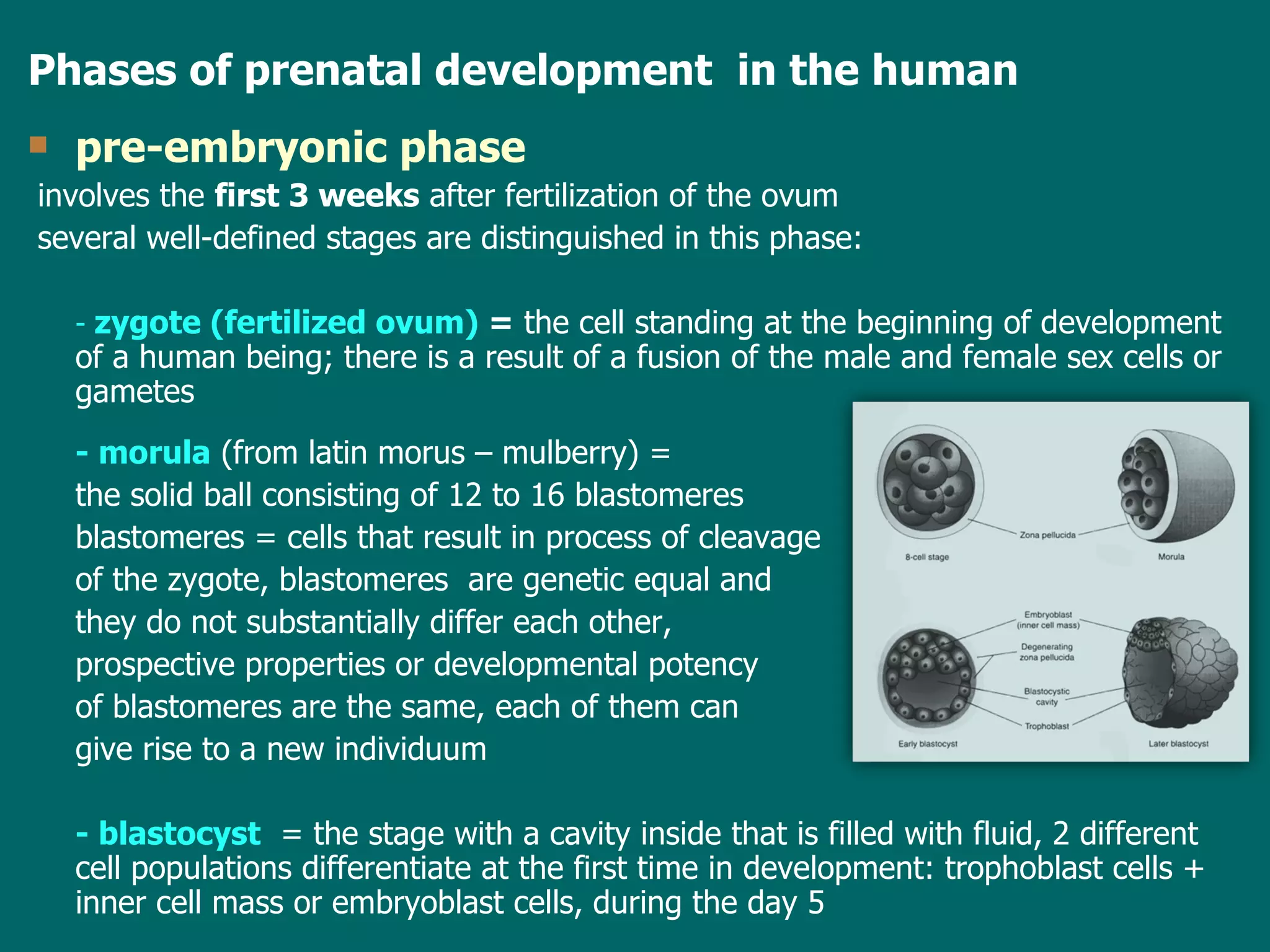
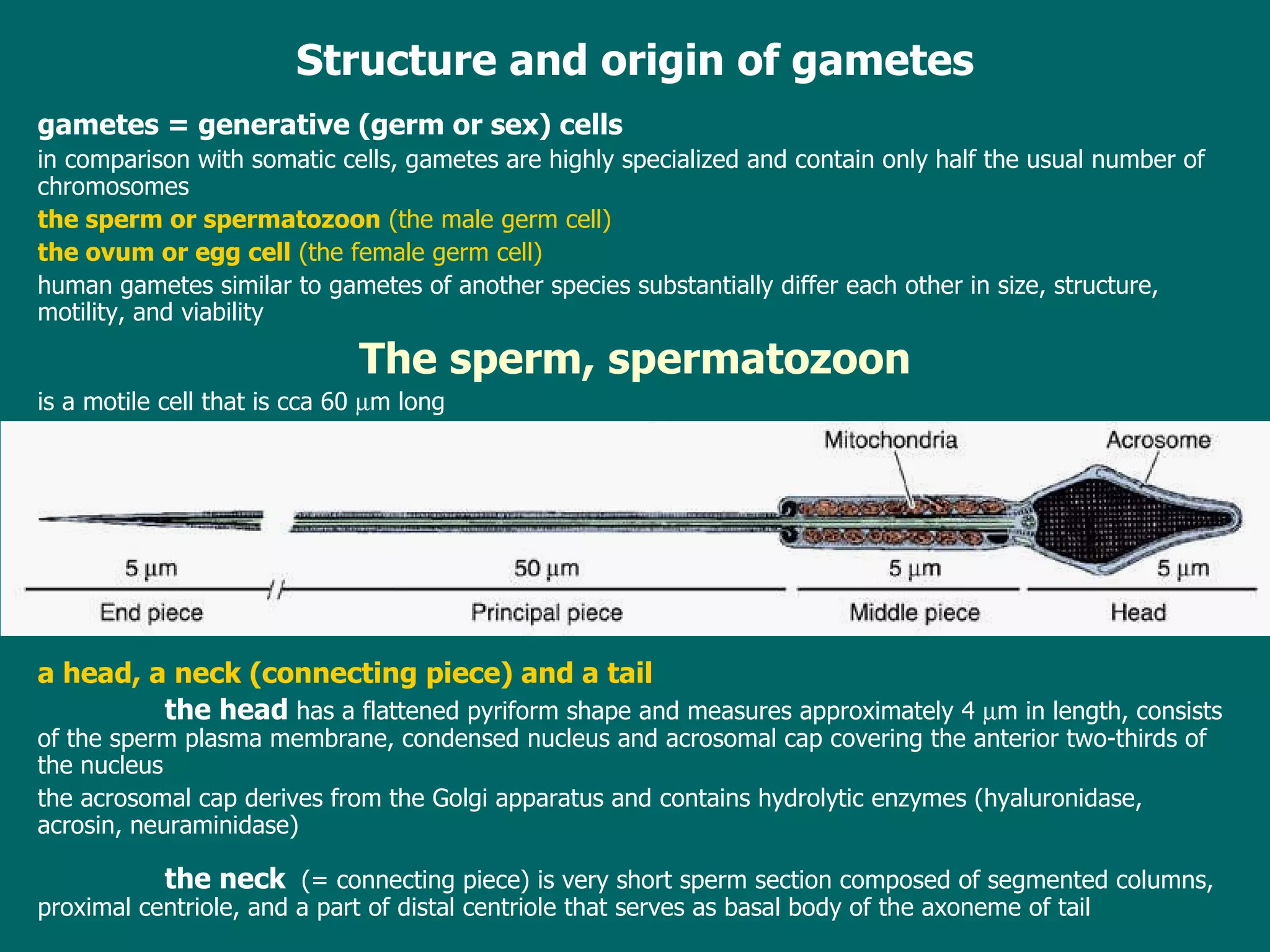
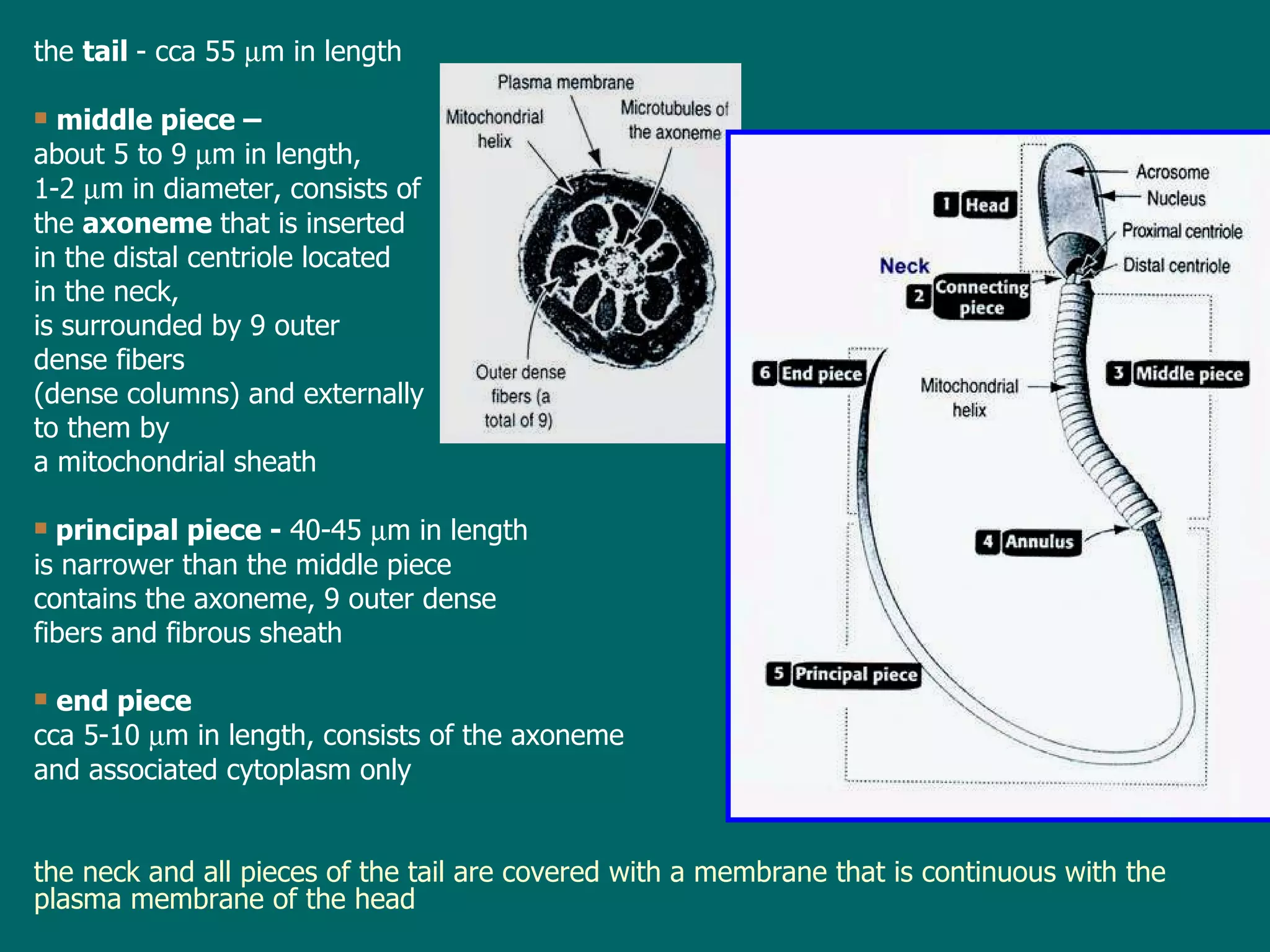
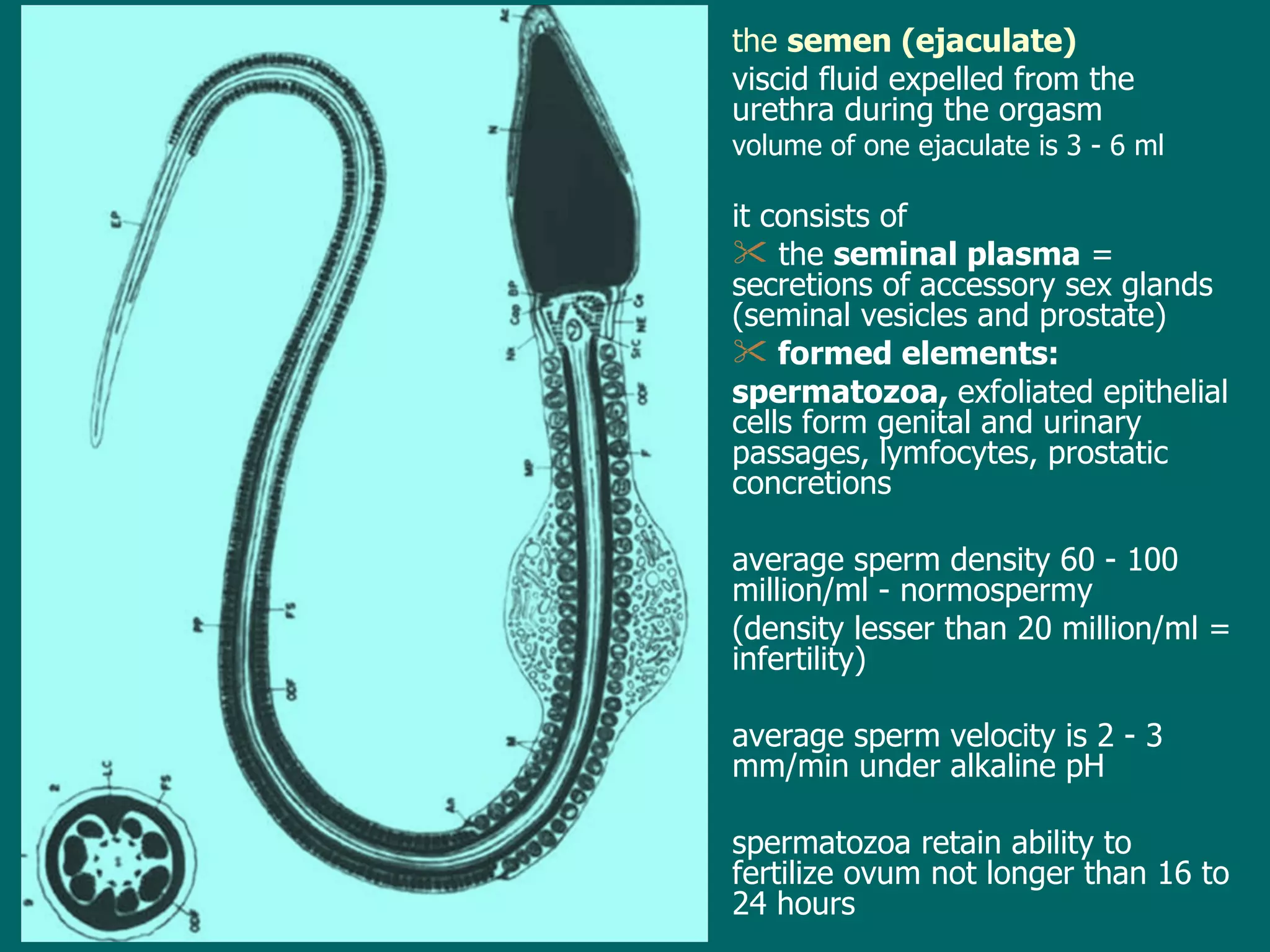
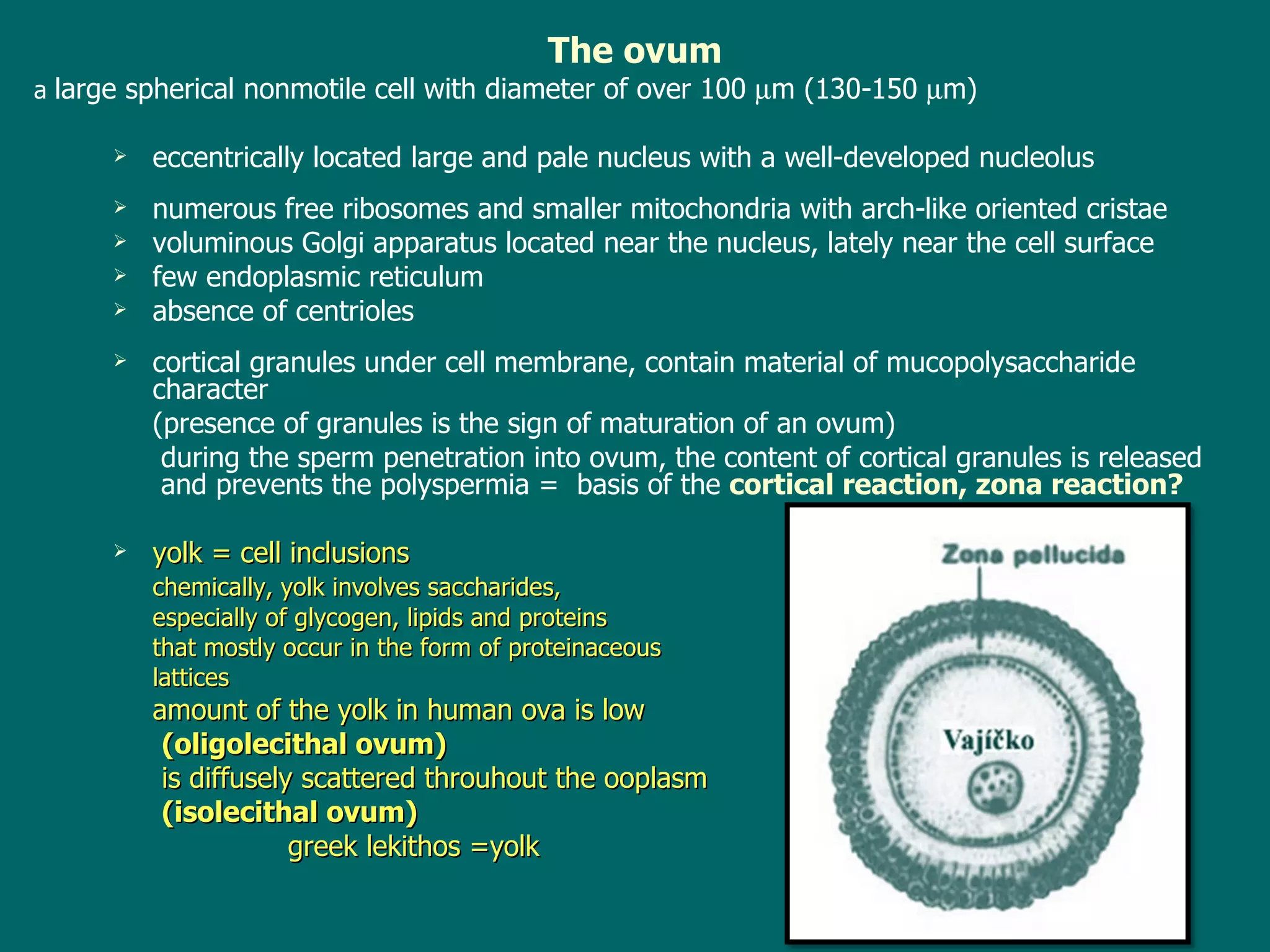
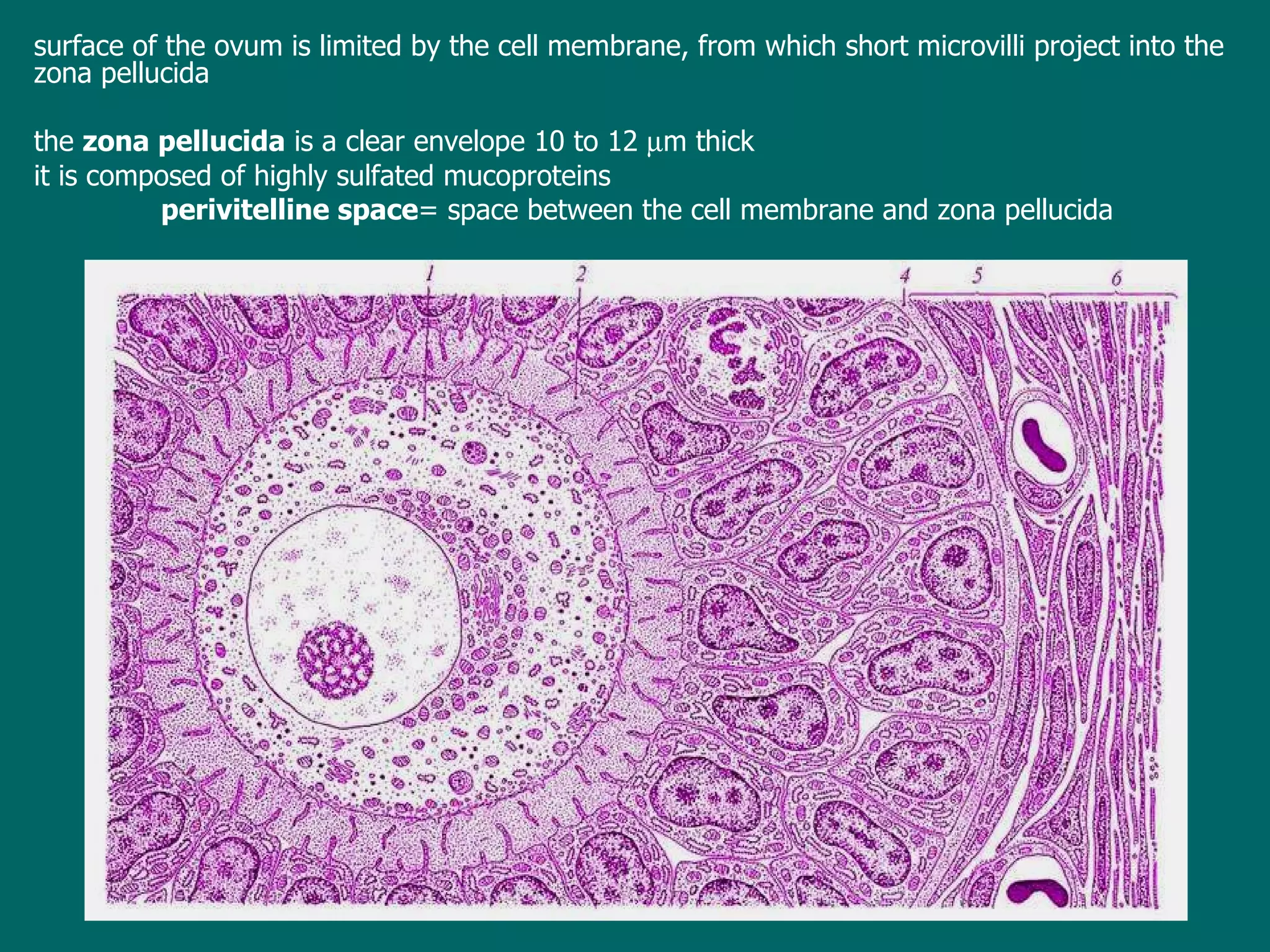
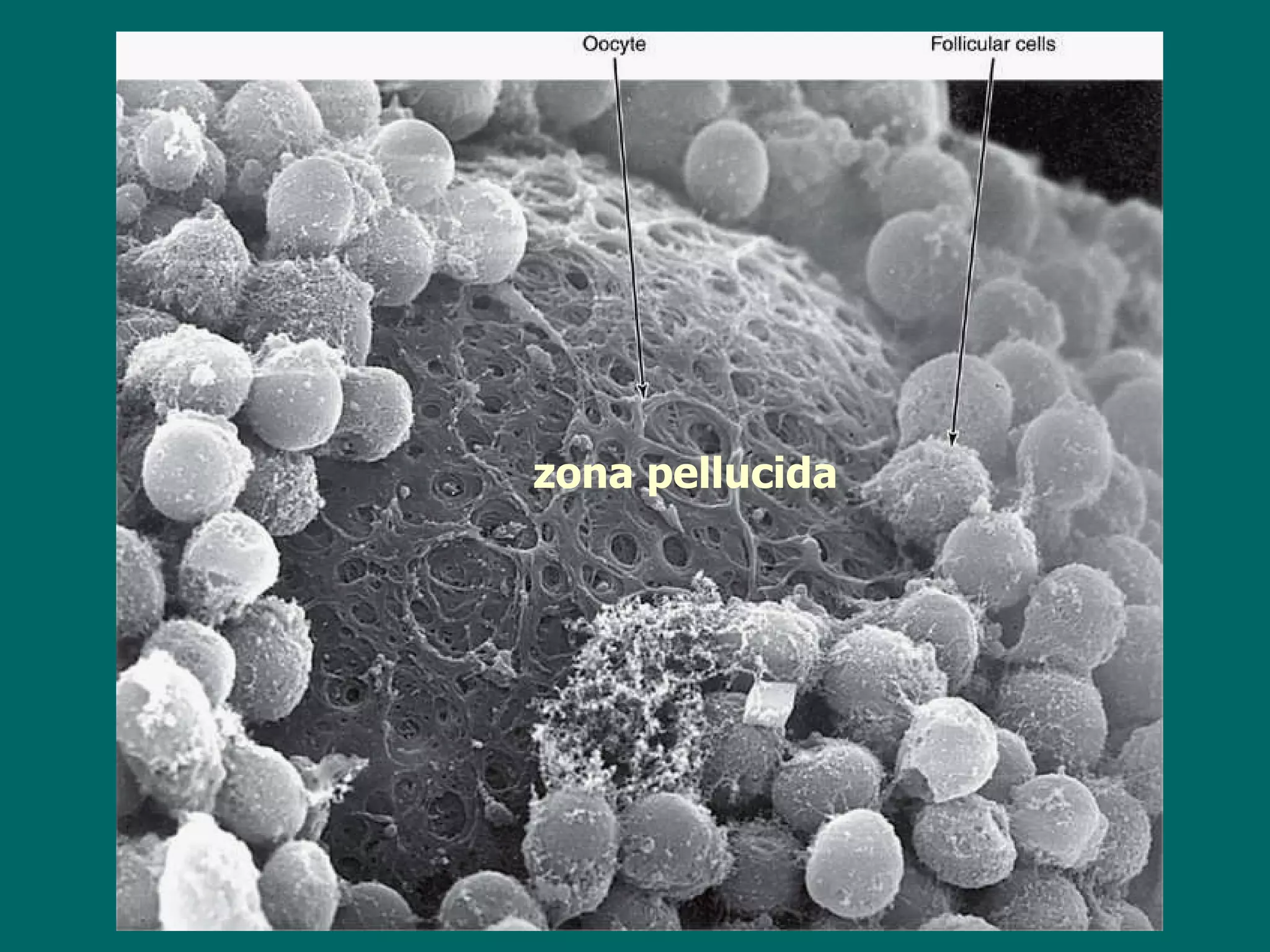
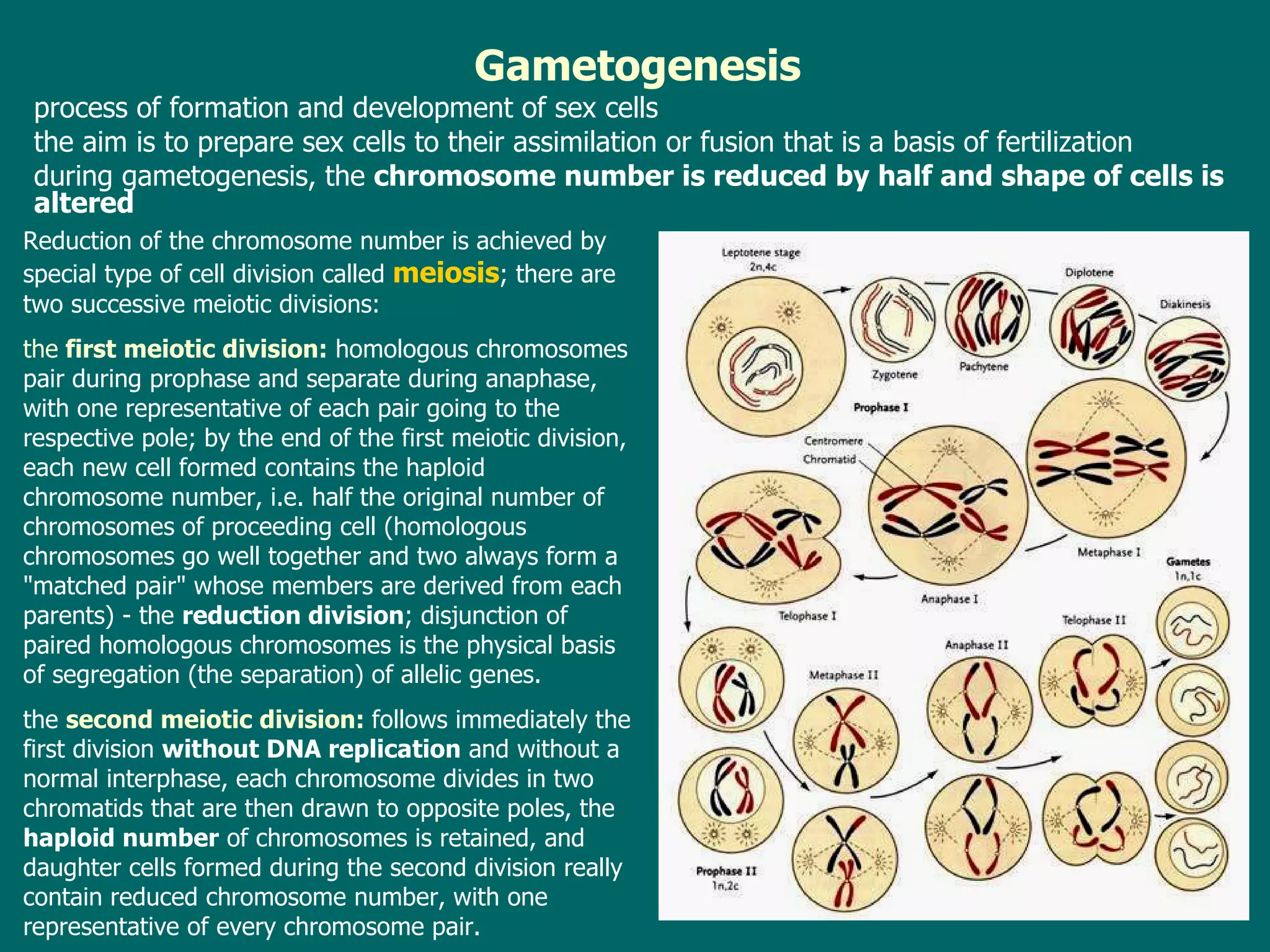
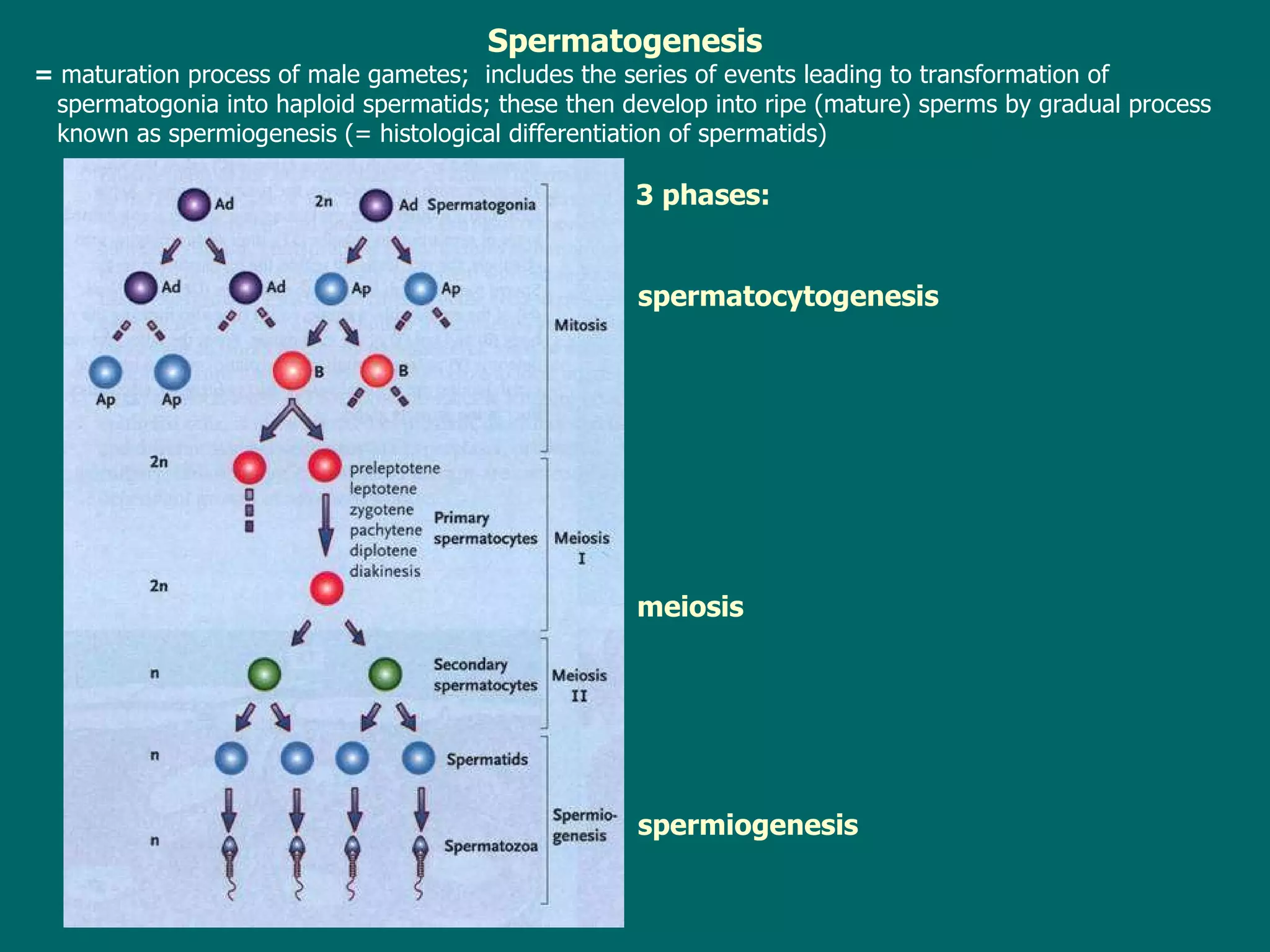
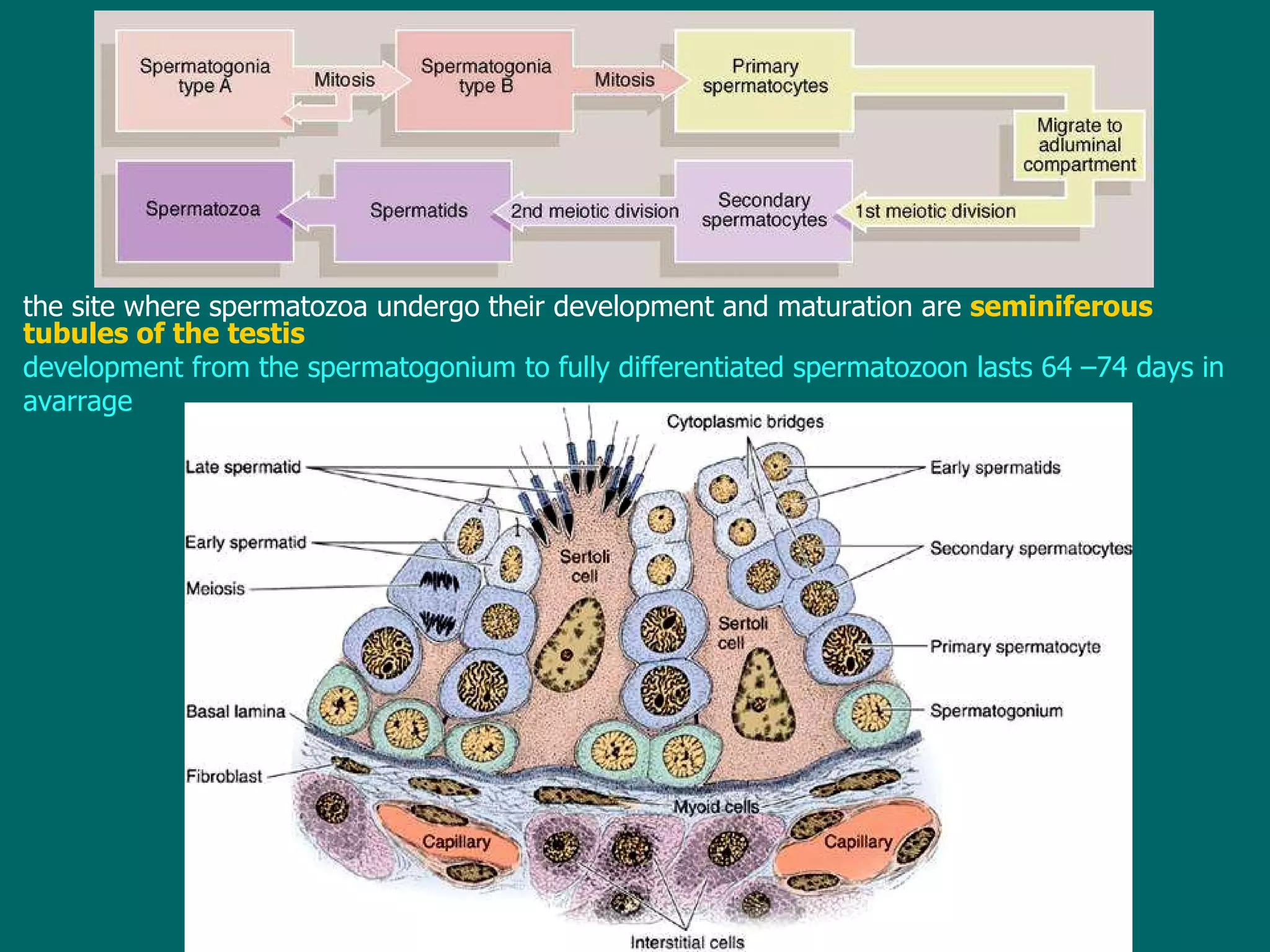
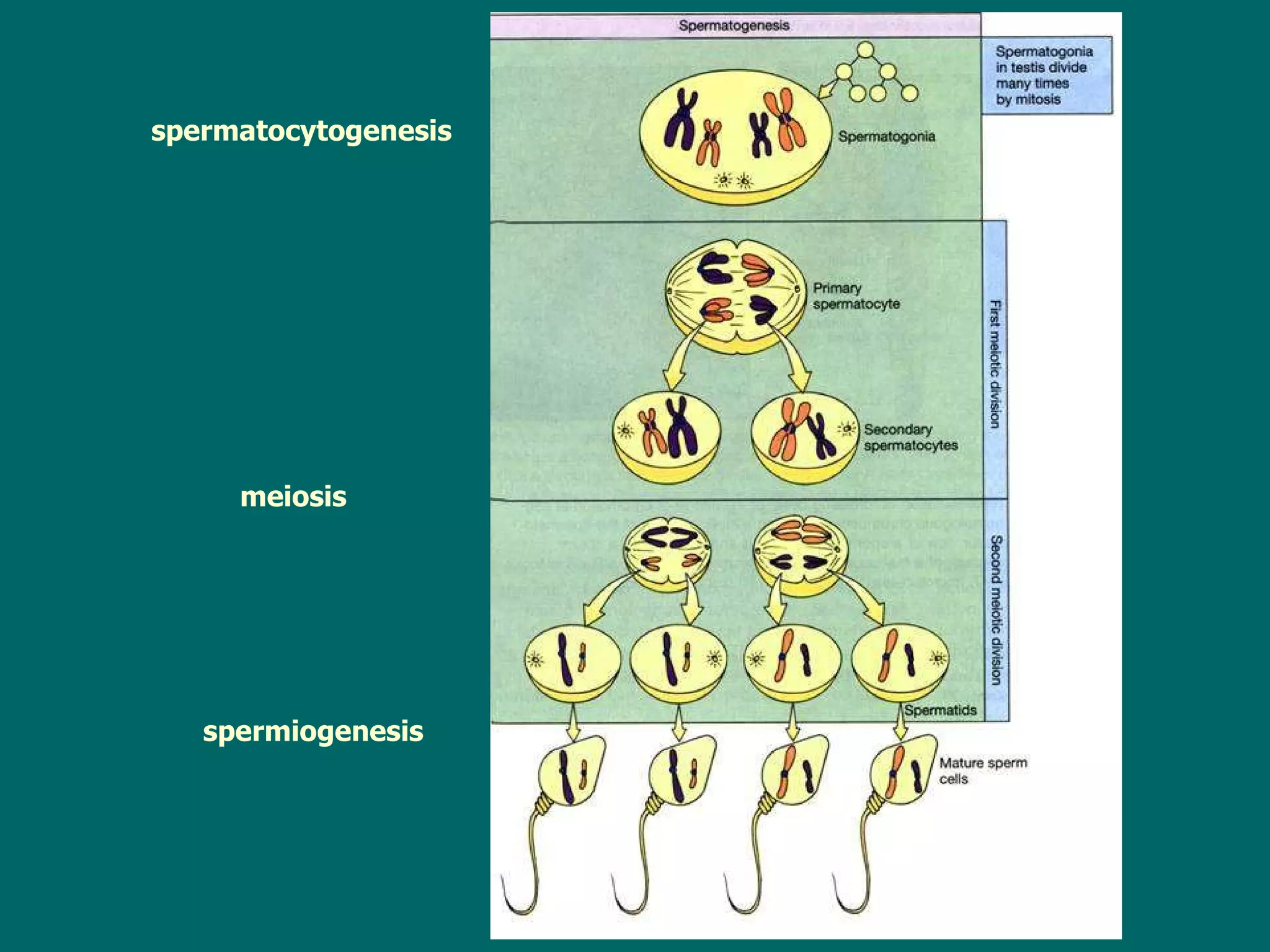
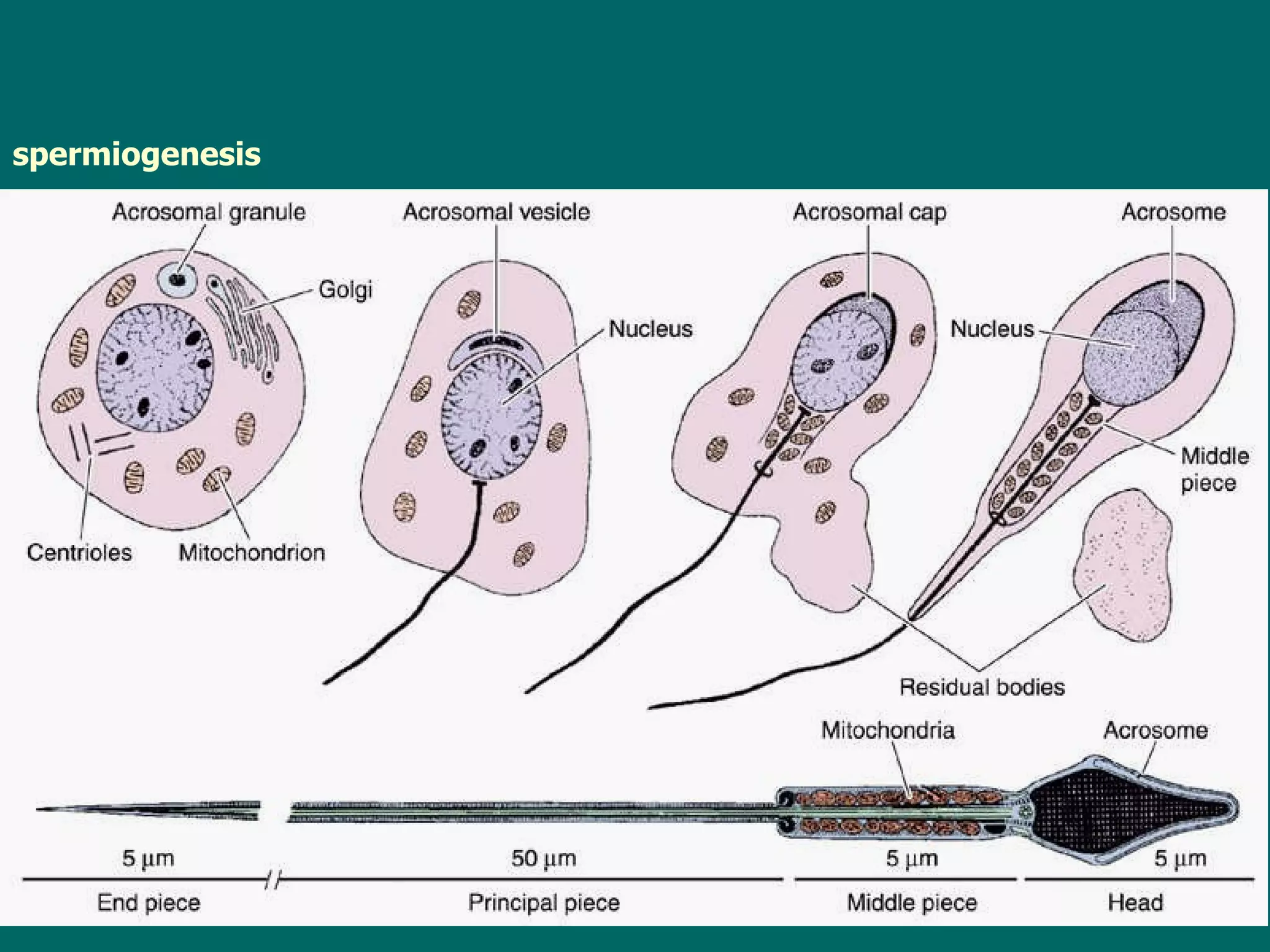
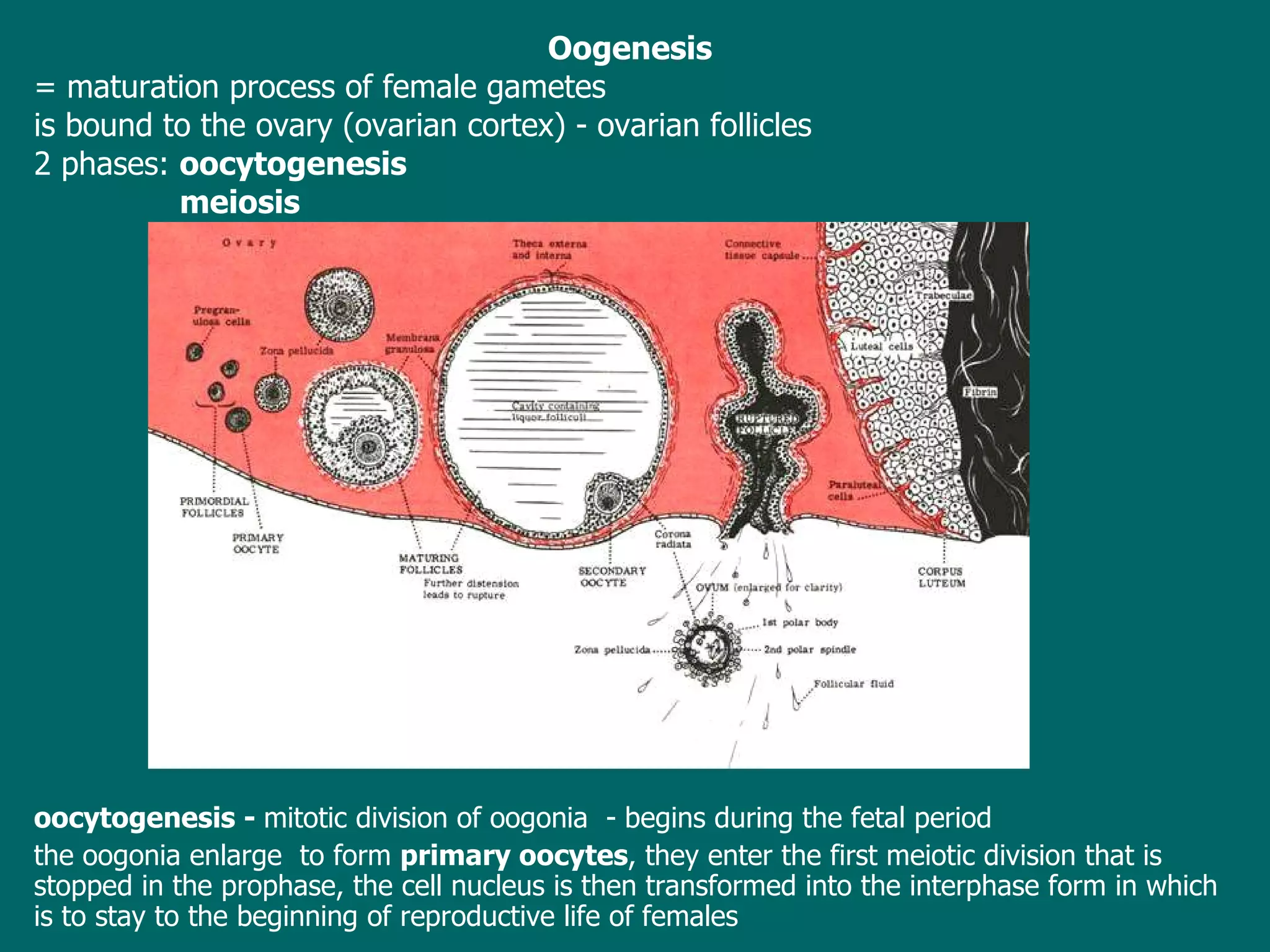
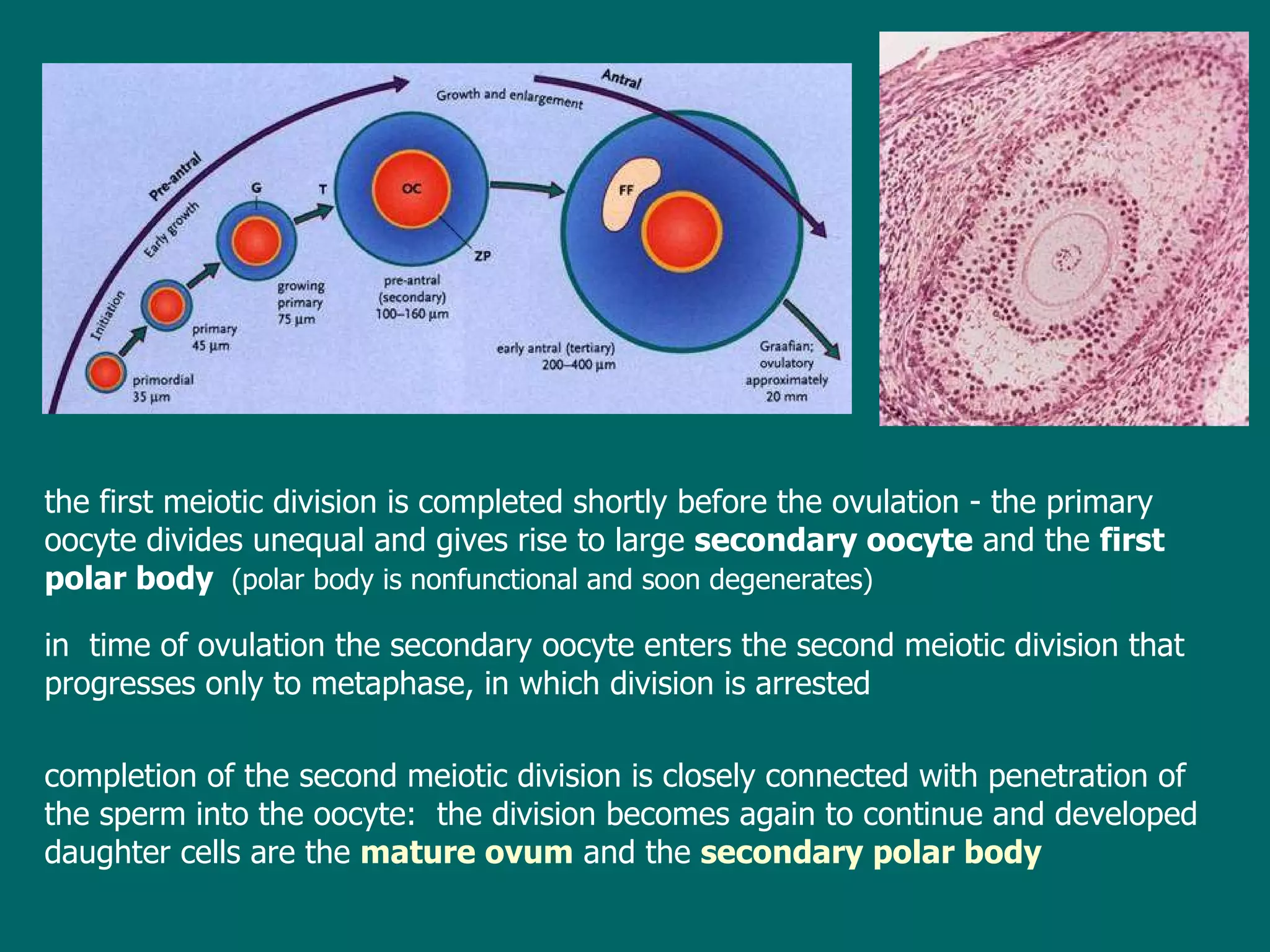
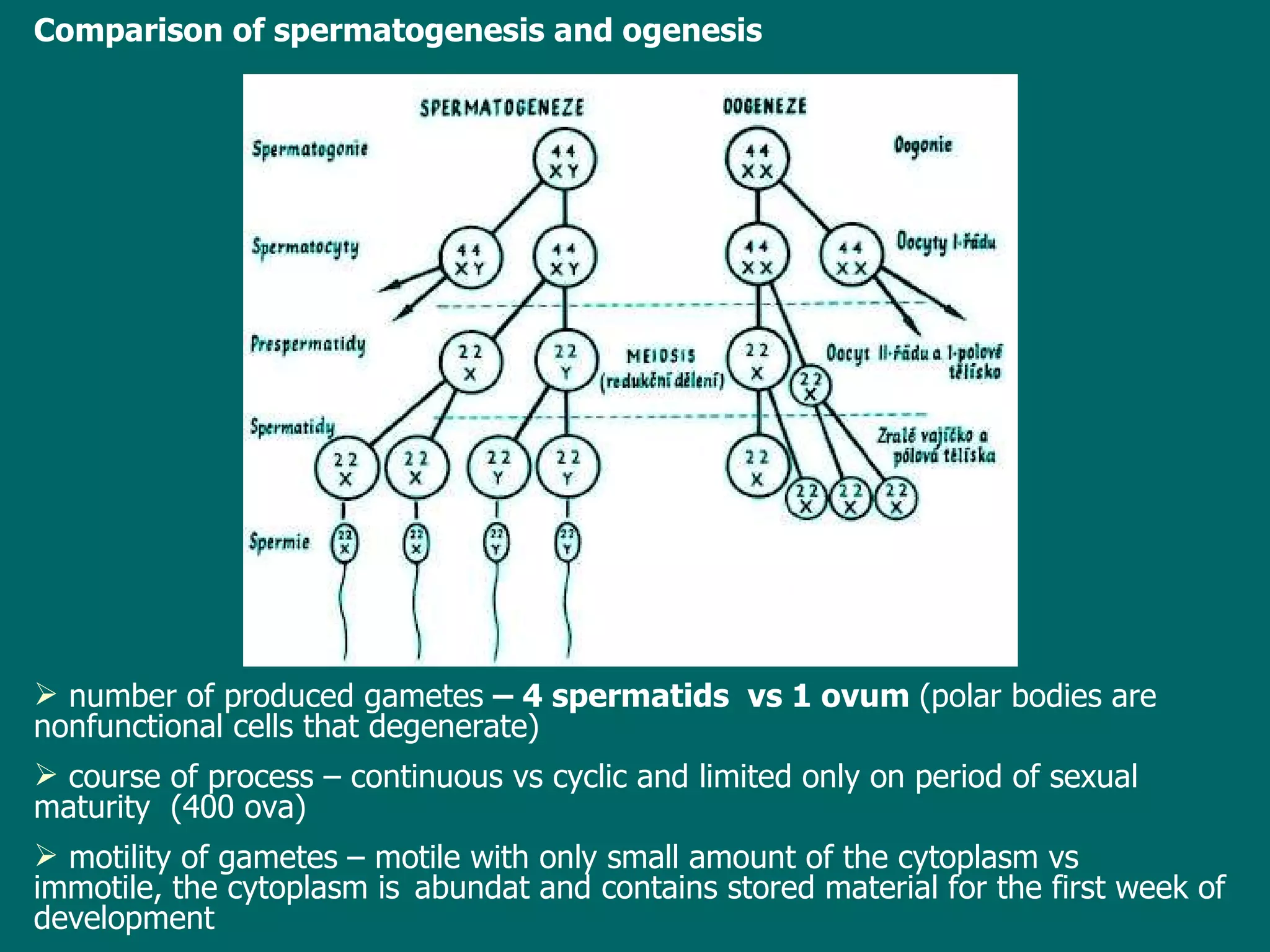
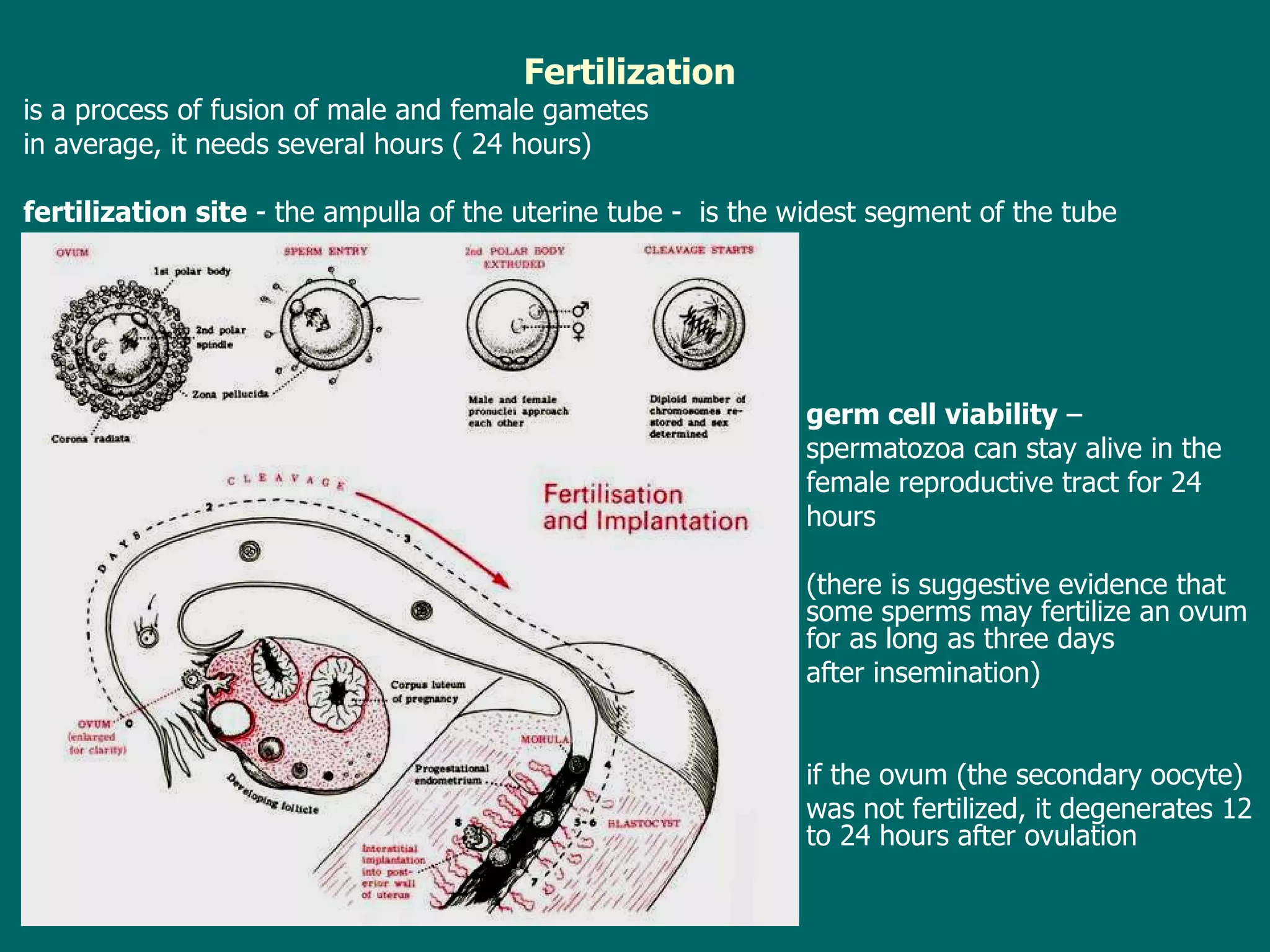
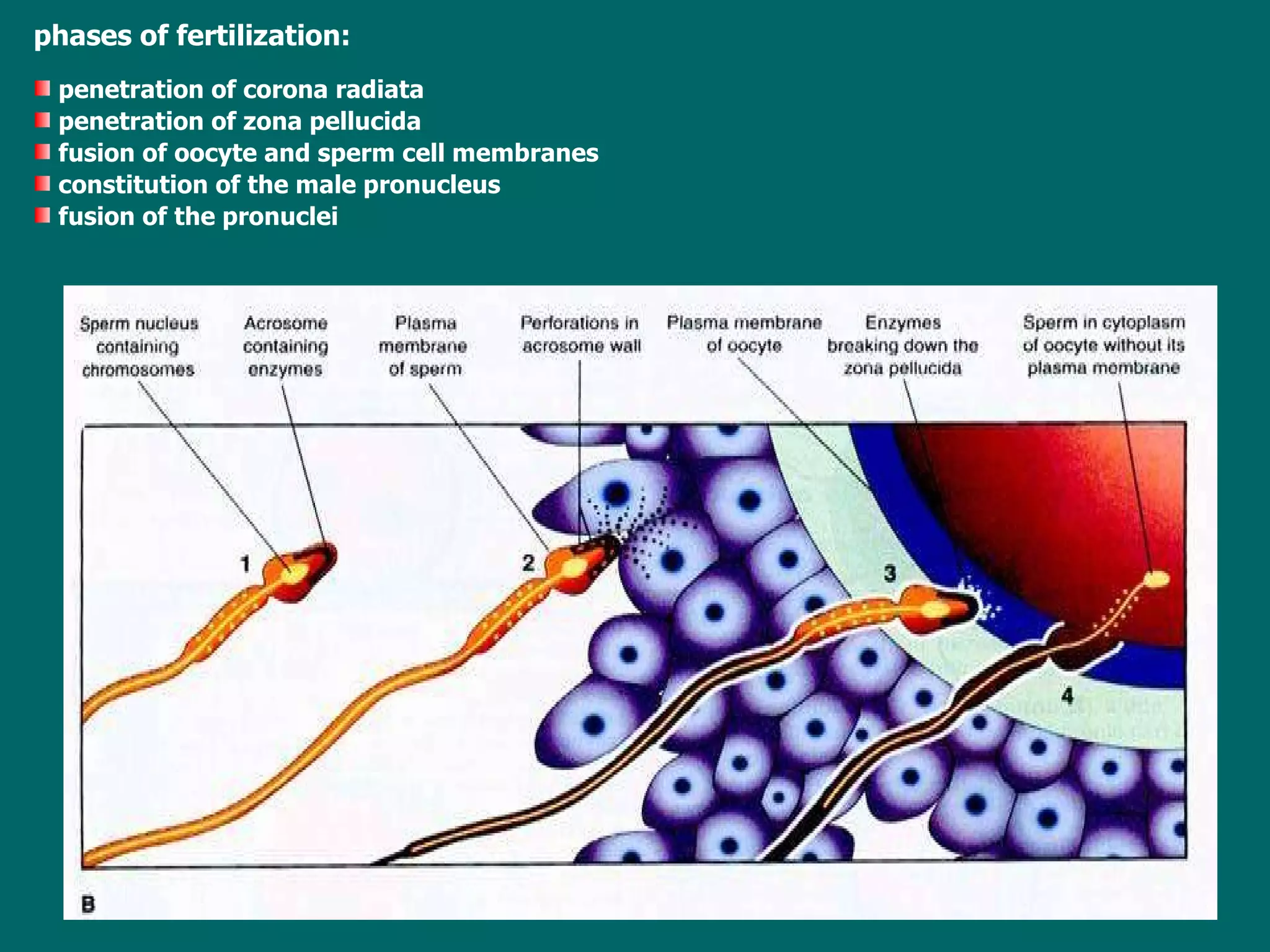
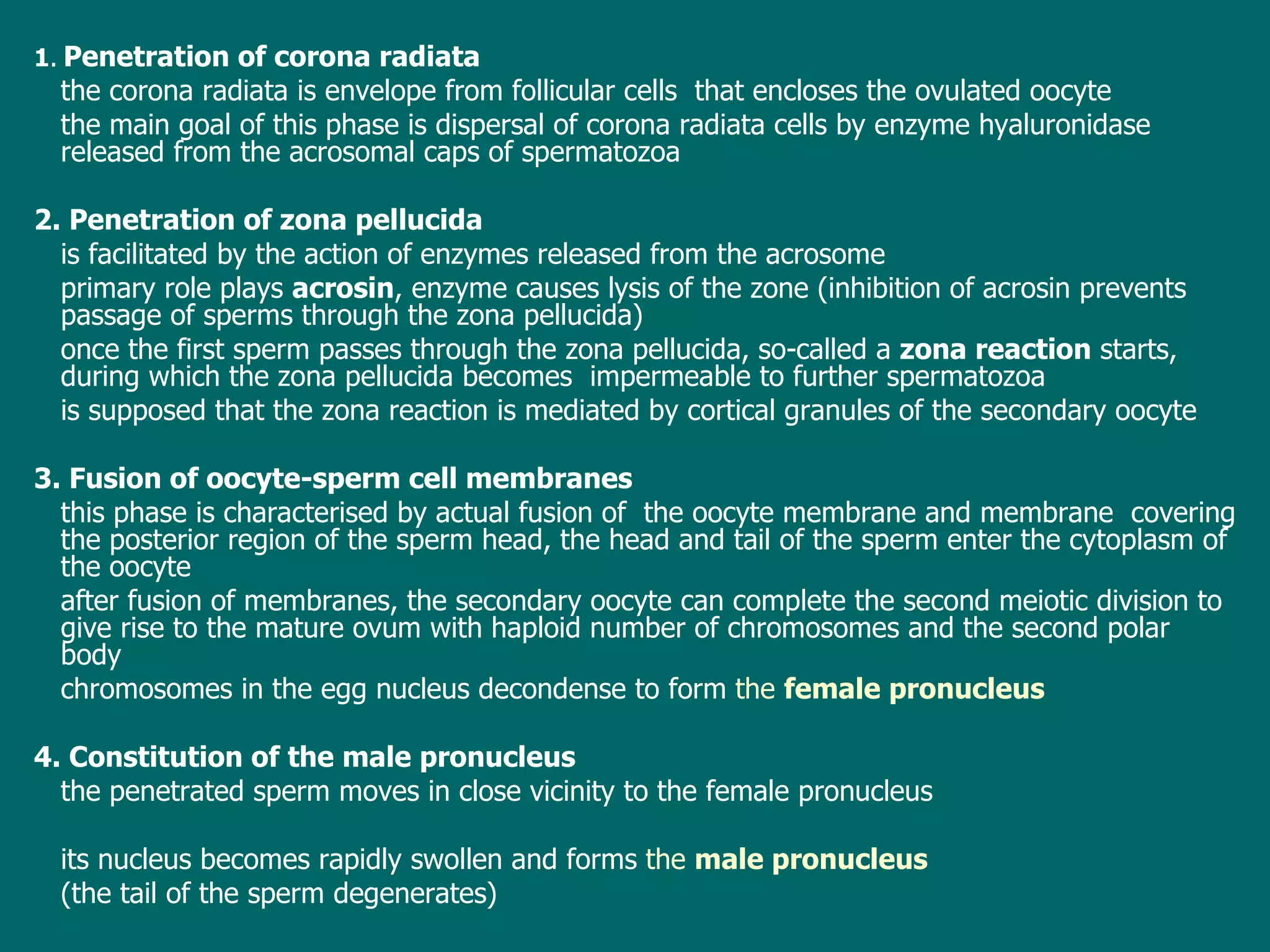
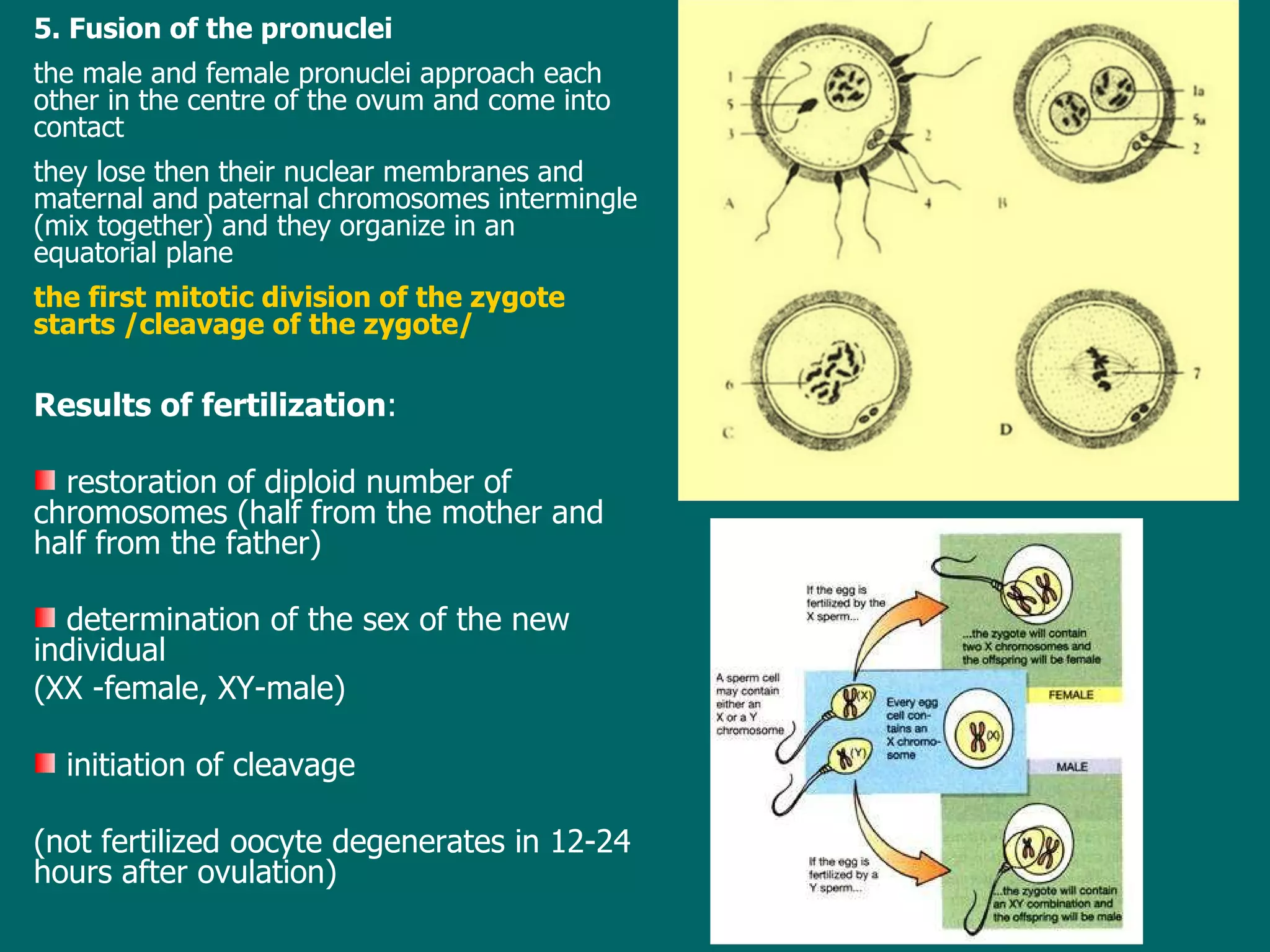
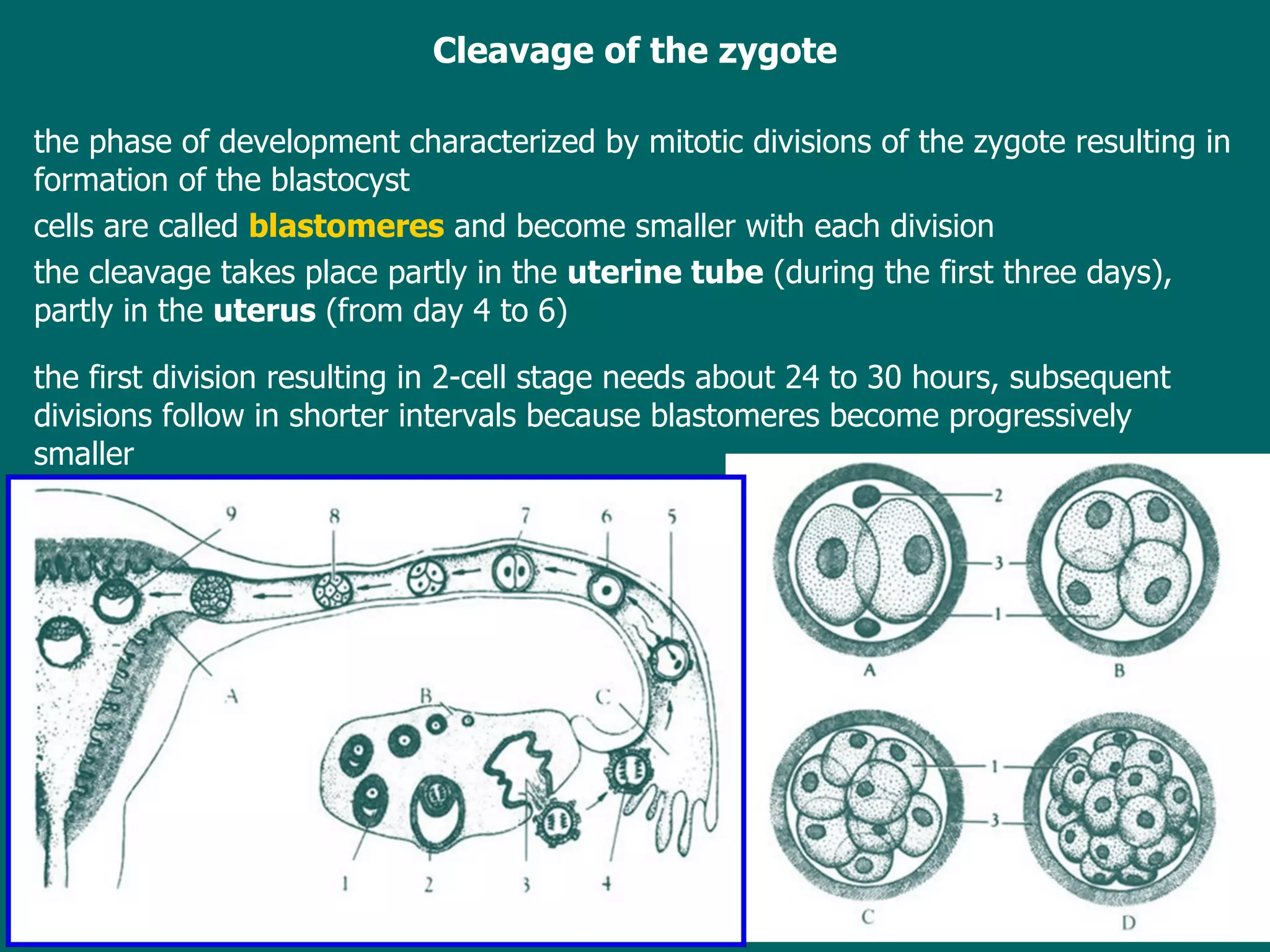
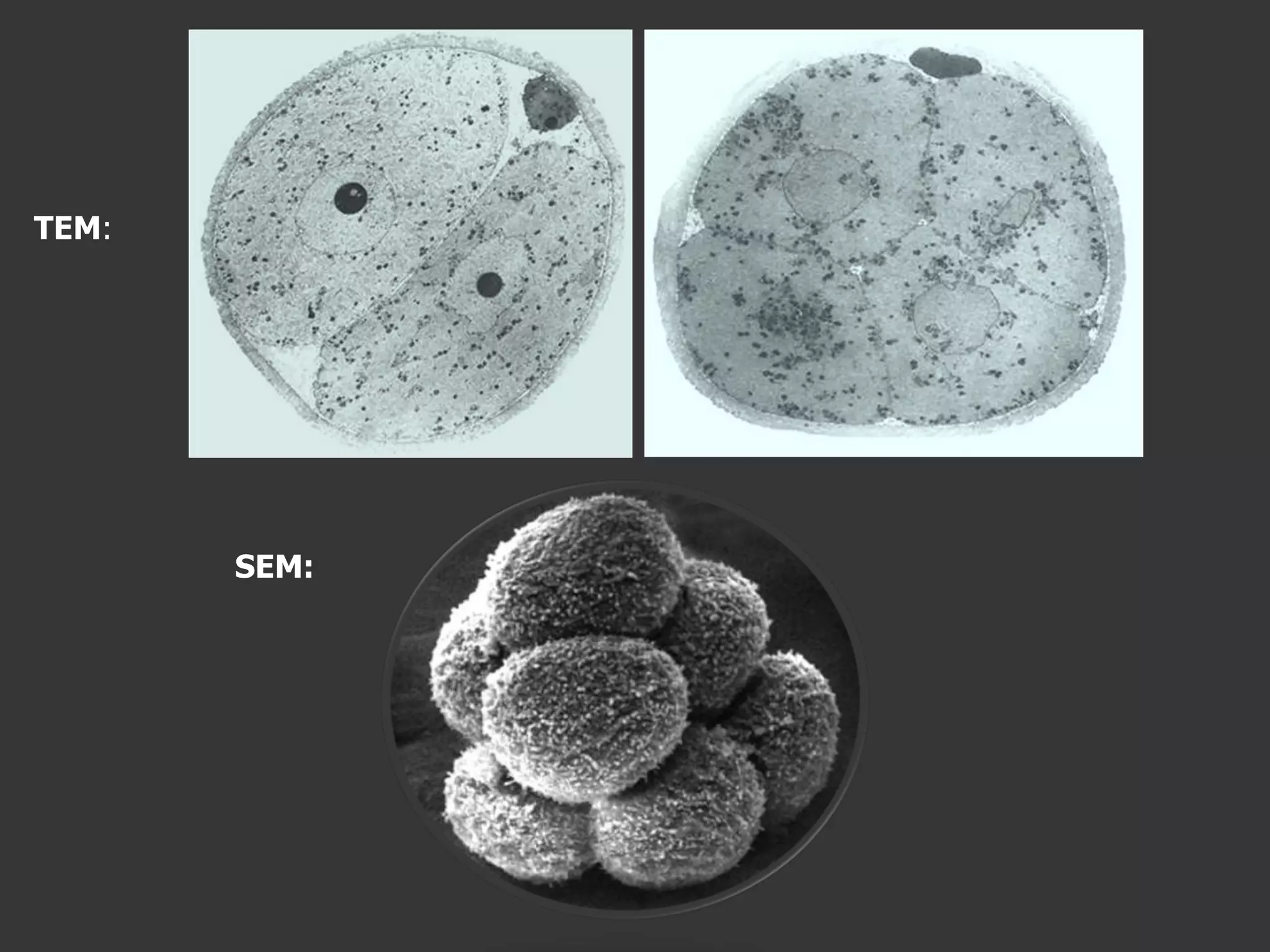
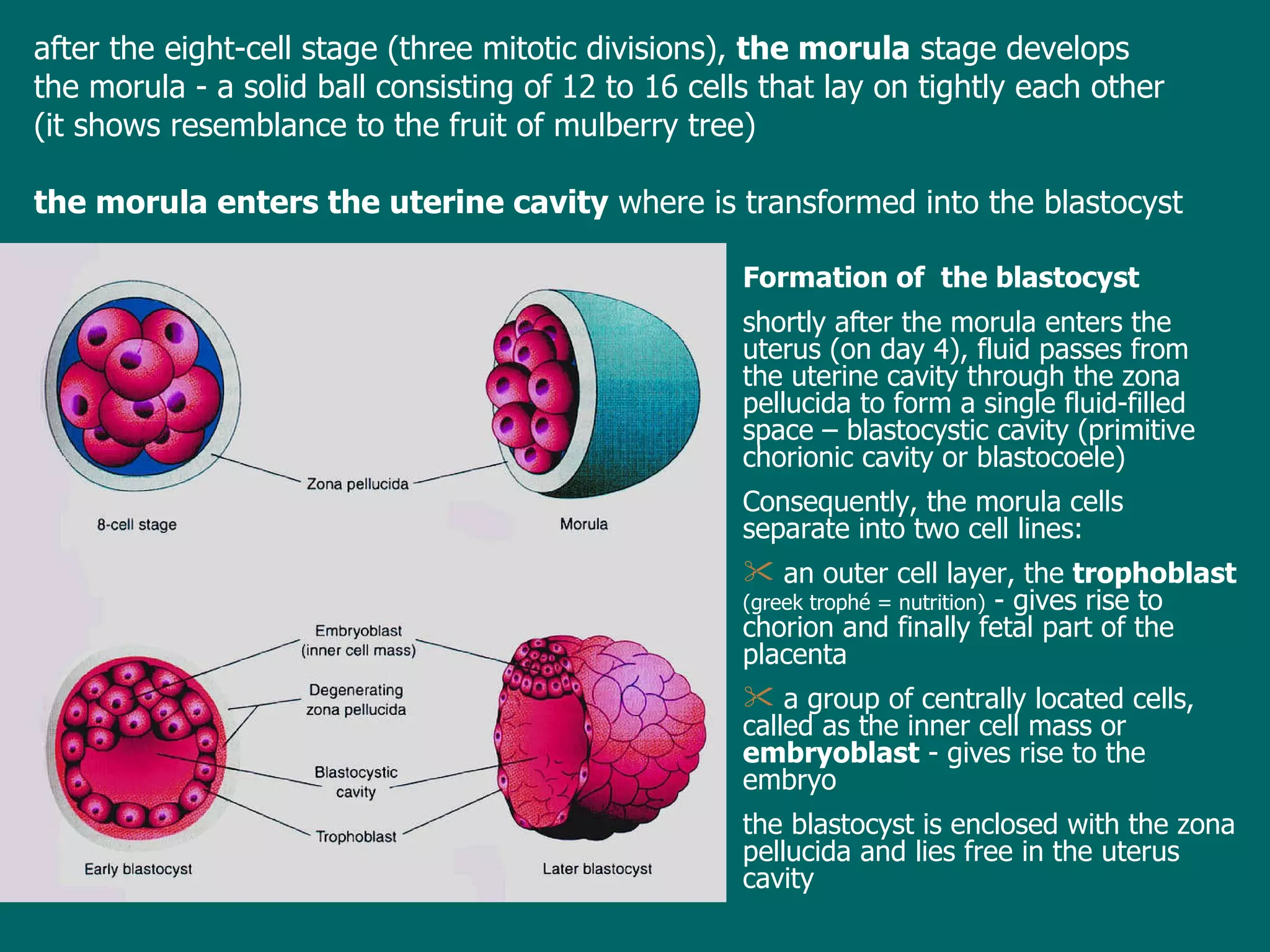
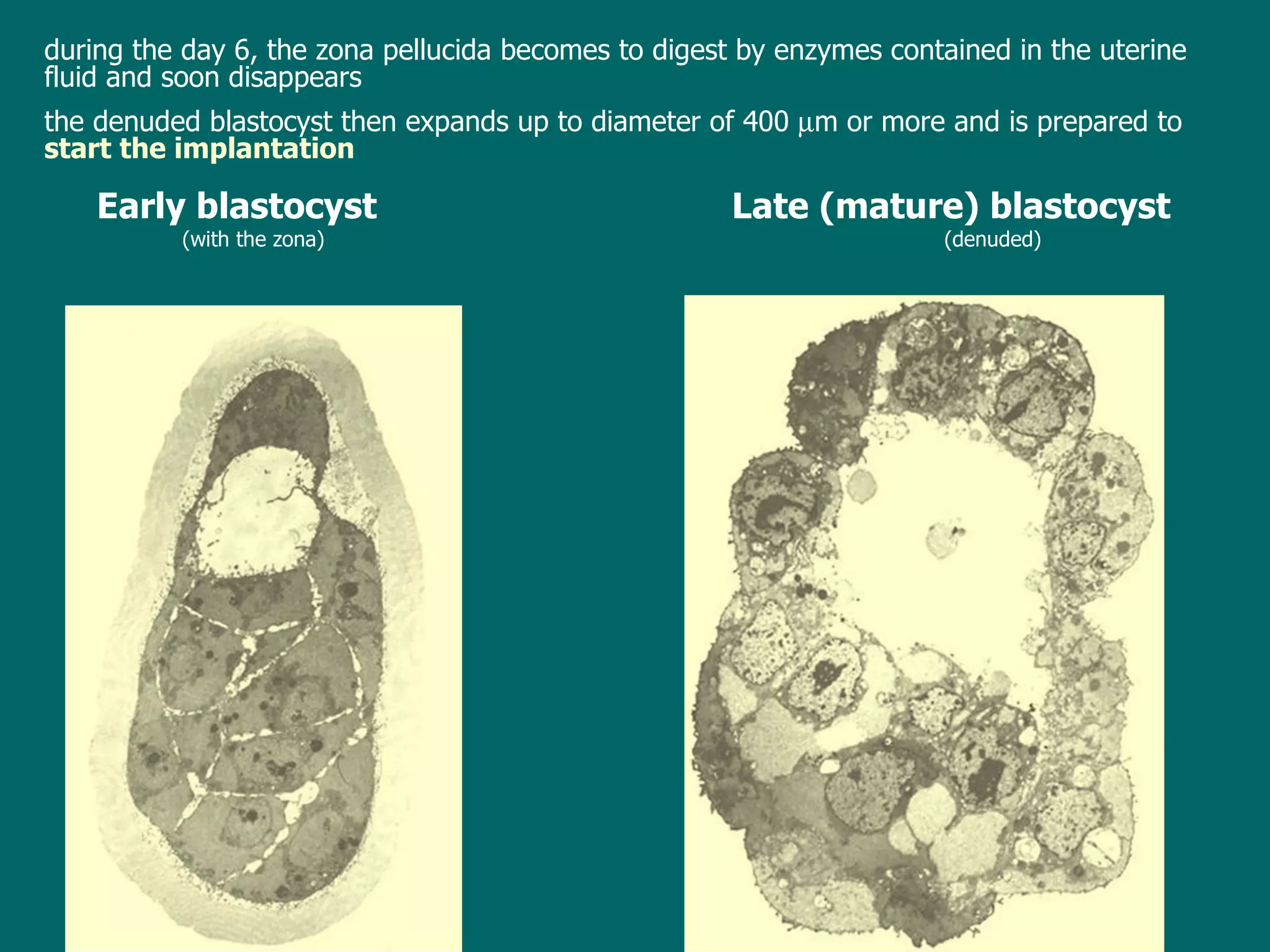
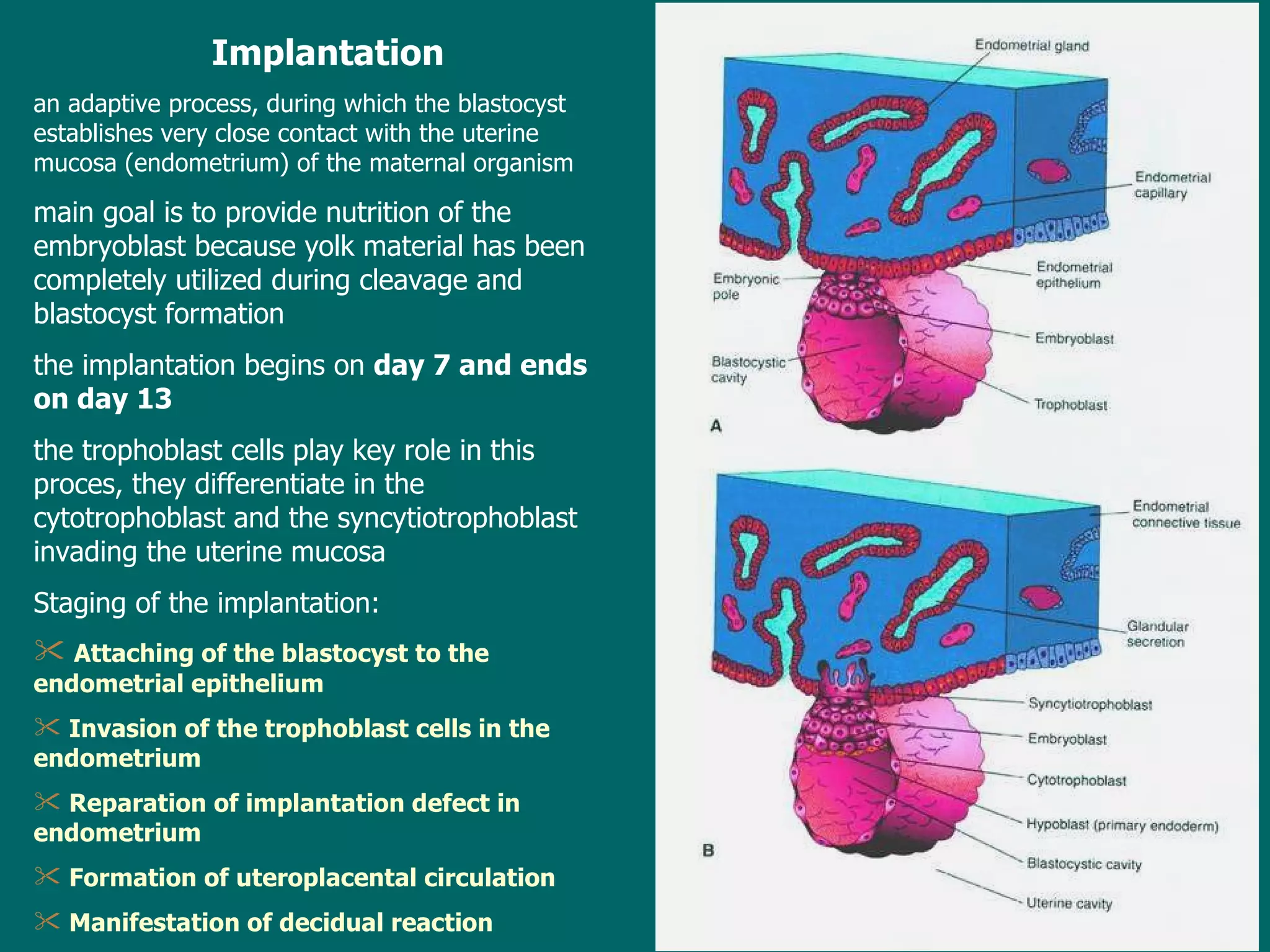
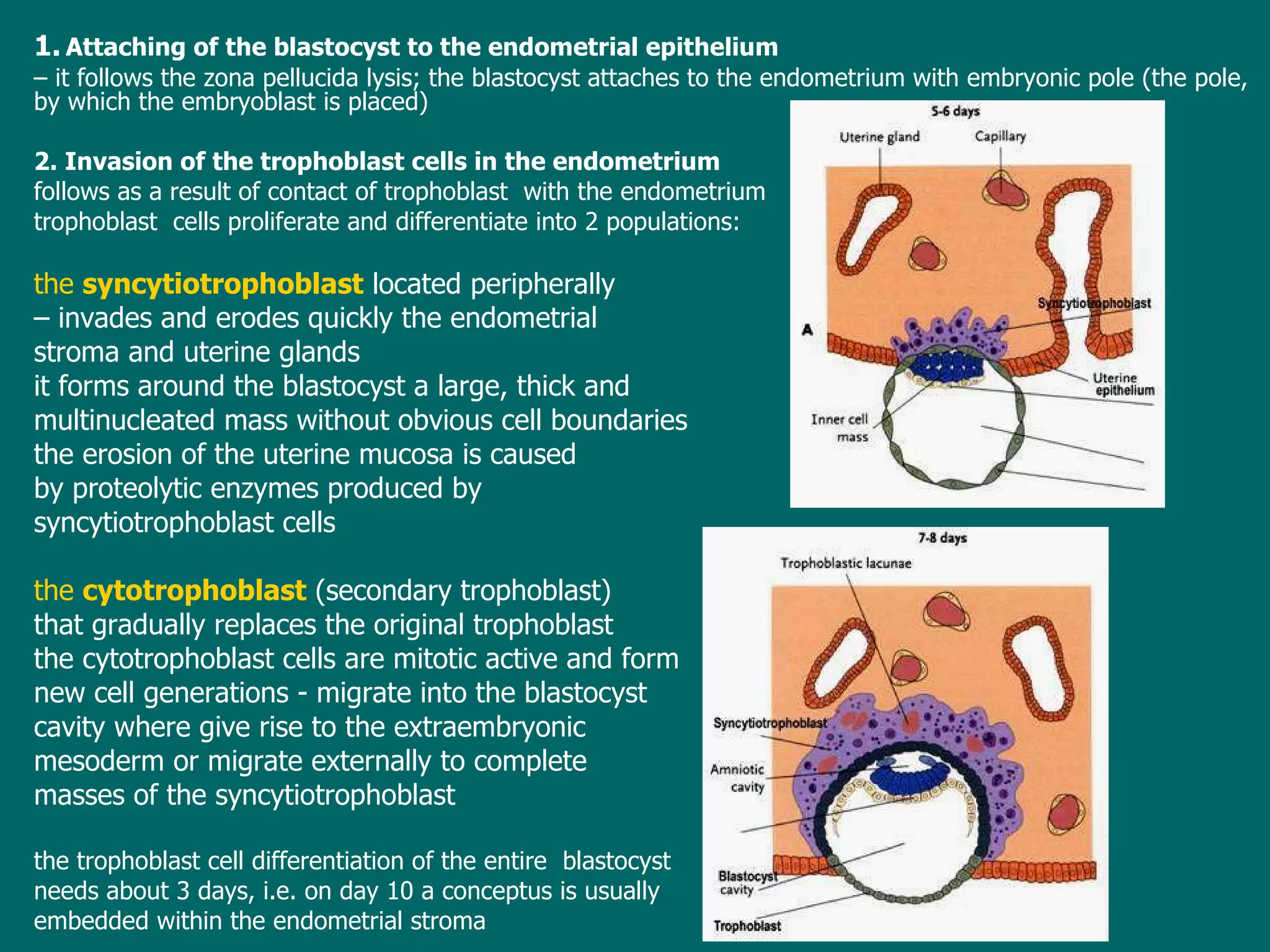
The document provides an overview of embryology, discussing key phases of human development from fertilization through birth. It describes gamete formation (spermatogenesis and oogenesis), the stages of pre-embryonic development (zygote, morula, blastocyst), and the prenatal and postnatal developmental periods. The structure and origin of male and female gametes are also summarized.