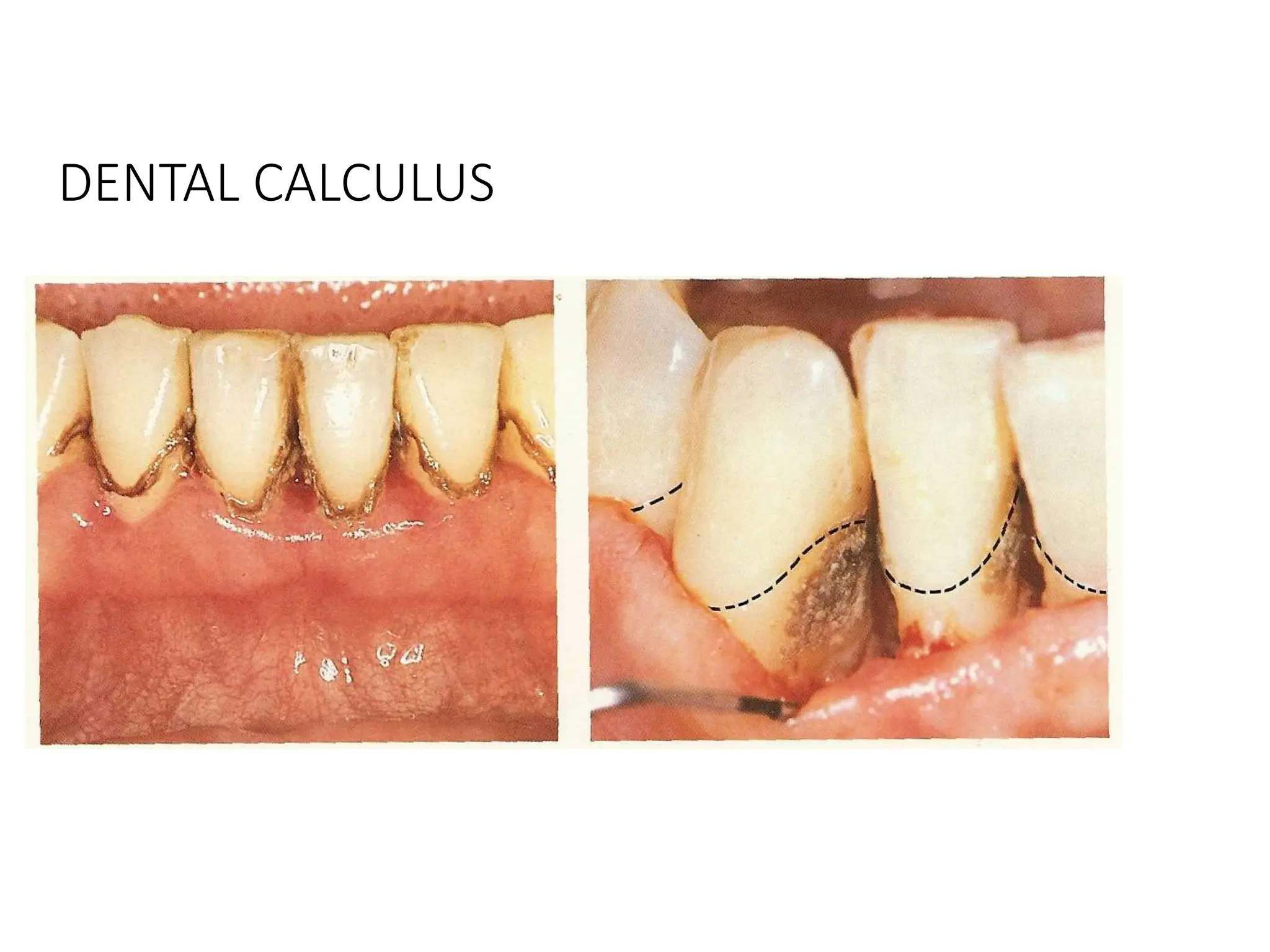
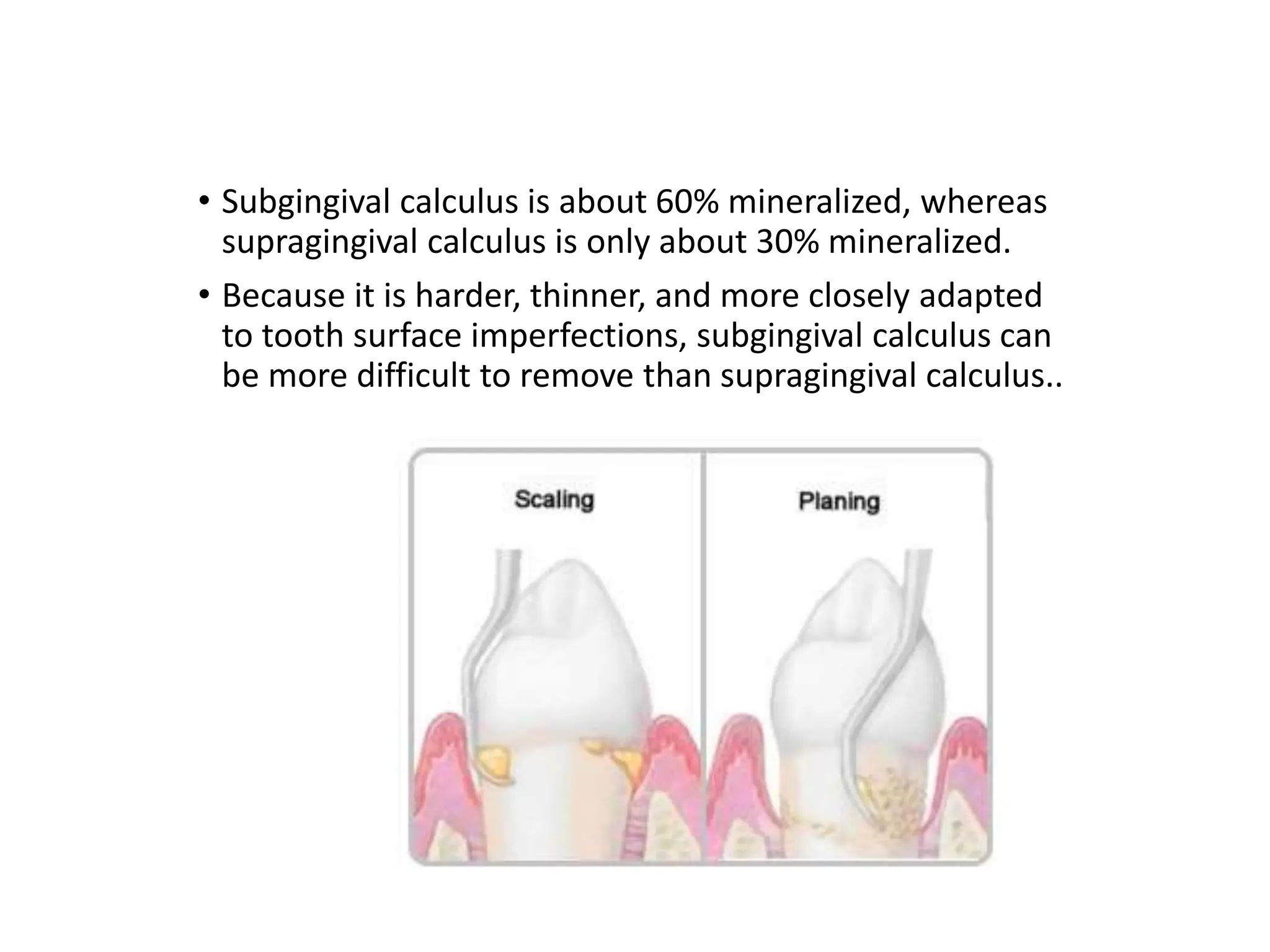
Dental calculus is a mineralized dental biofilm that forms on teeth and dental prostheses, significantly contributing to inflammatory periodontal disease by harboring bacteria close to gingival tissue. It is classified as supragingival or subgingival based on its location related to the gingival margin, and the formation of calculus involves pellicle formation, biofilm maturation, and mineralization. The control of biofilm and calculus is crucial for reducing gingival inflammation and for effective patient education on treatment and prevention strategies.