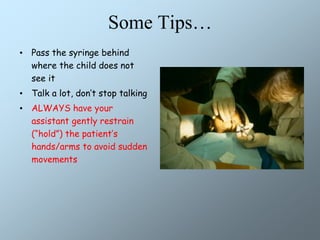
This document discusses behavior management techniques and local anesthesia when treating children in a dental setting. It outlines objectives of ensuring procedures are performed efficiently, safely, and instilling a positive attitude in children. Both pharmacological and non-pharmacological techniques are described, including sedation, general anesthesia, restraint, and behavior management using distraction, positive reinforcement, and parental absence. The document provides guidance on communication skills like reflective listening and descriptive praise to help anxious children. It also reviews local anesthetic properties, complications, maximum dosing calculations, and tips for making injections less painful.