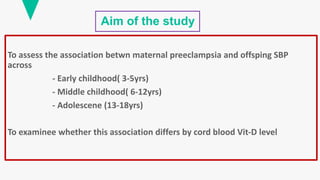
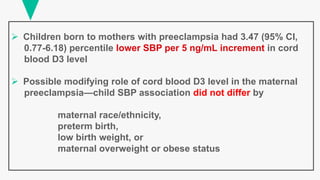
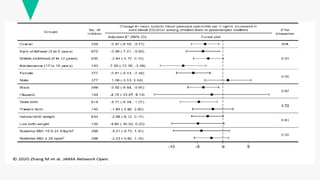
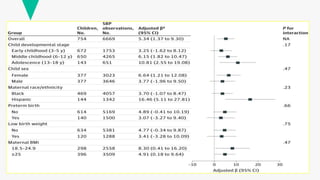
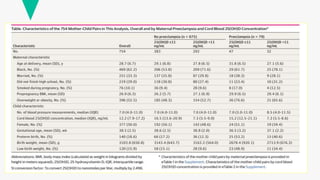
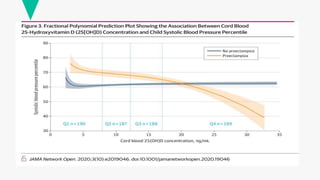
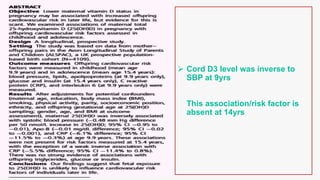
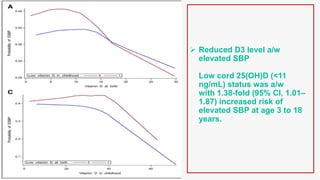
Maternal preeclampsia is associated with higher childhood blood pressure from ages 3 to 18 years. This association varies by cord blood vitamin D levels. Children born to mothers with preeclampsia had higher blood pressure if their cord blood vitamin D was below 11 ng/mL. However, for every 5 ng/mL increase in cord blood vitamin D, these children had 3.47 percentile lower blood pressure. Higher cord blood vitamin D may modify the relationship between maternal preeclampsia and offspring blood pressure.