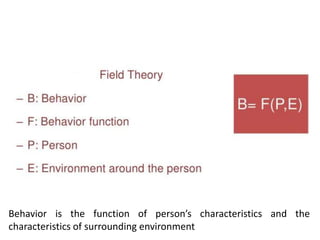
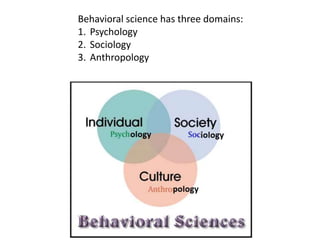
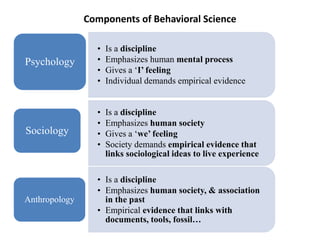
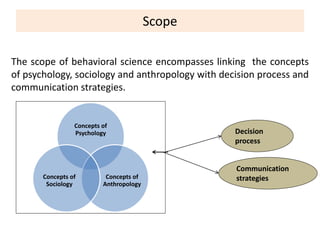
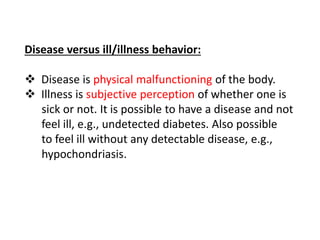
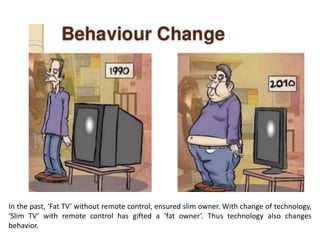
1. Behavioral science is the study of human behavior through the lenses of psychology, sociology, and anthropology. It examines how individuals and groups act, think, and make decisions.
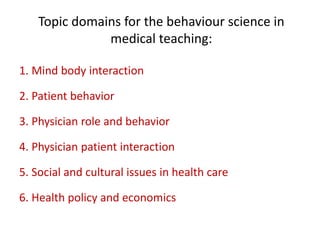
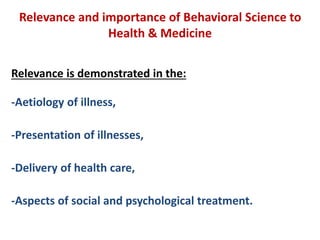
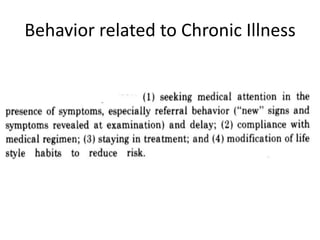
2. Understanding behavioral science is important for healthcare as it provides insights into patient behaviors, physician-patient interactions, and social and cultural factors that influence health and healthcare delivery.
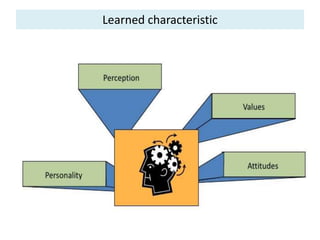
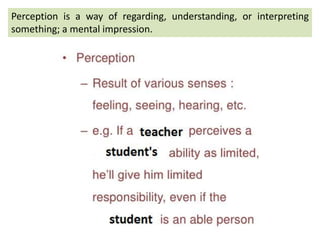
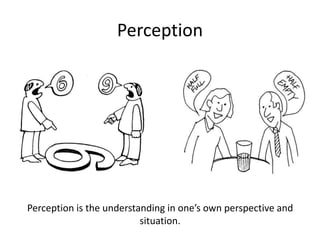
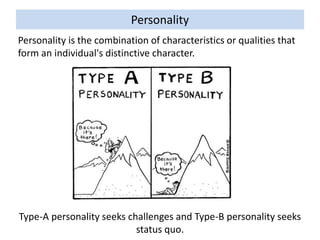
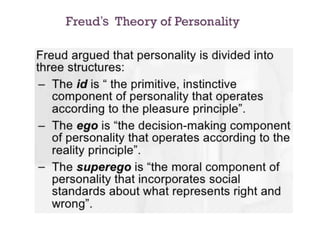
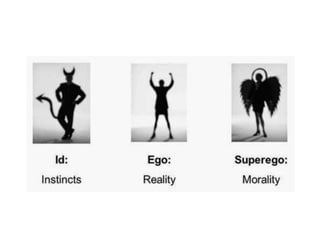
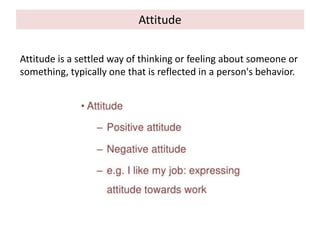
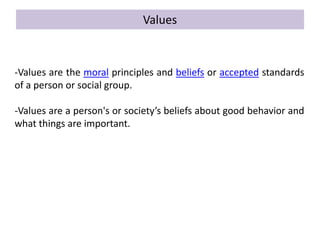
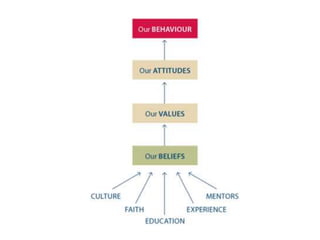
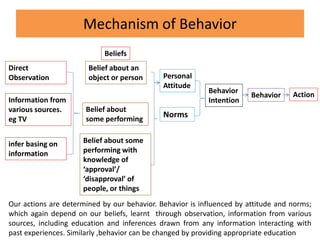
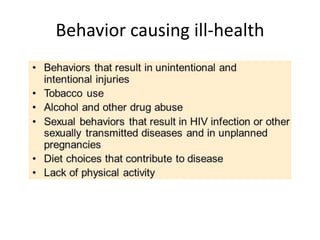
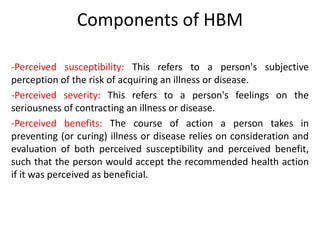
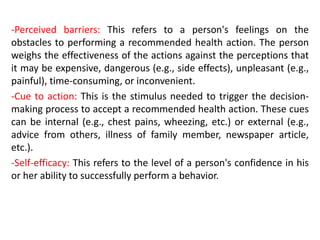
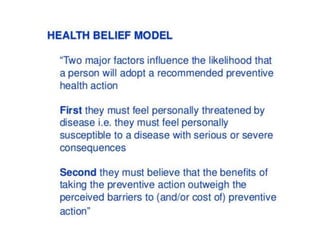
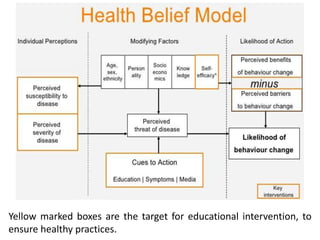
3. Applying concepts from behavioral science such as perception, attitudes, values, and decision-making can help healthcare providers develop effective strategies and recommendations to address patient risk factors and health conditions.