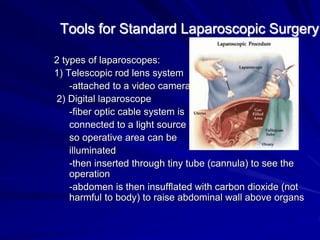
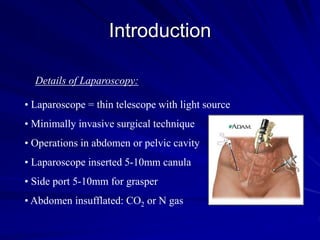
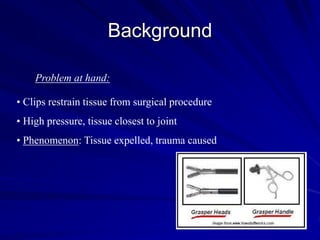
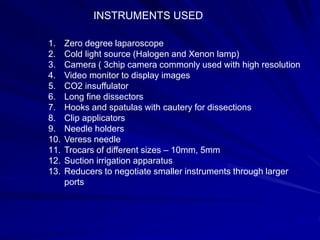
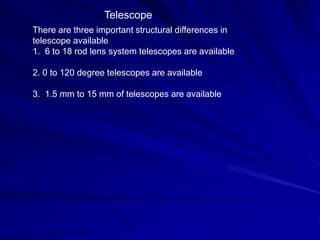
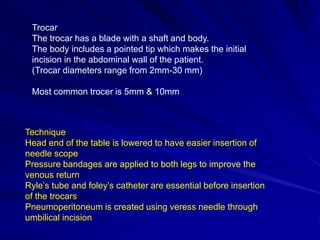
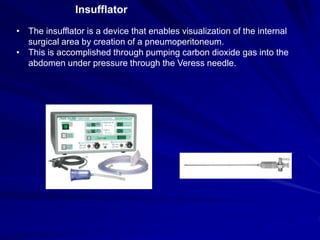
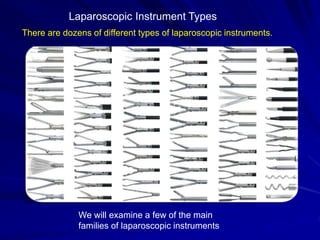
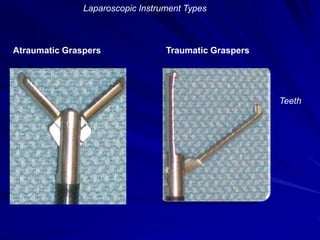
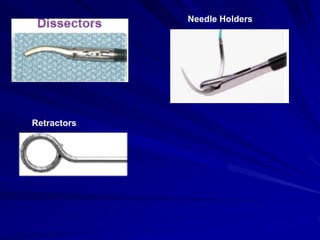
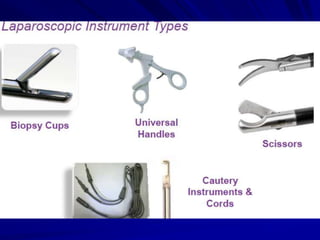
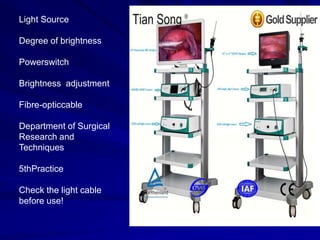
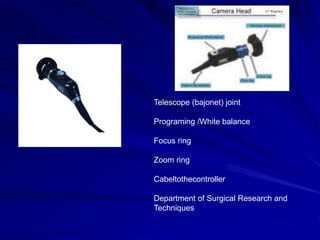
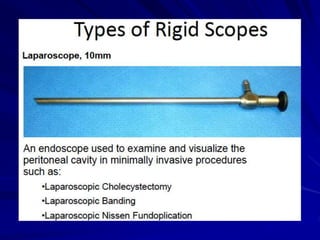
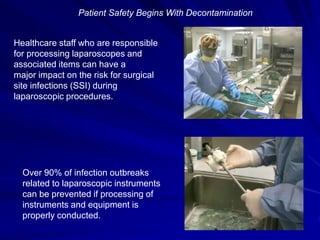
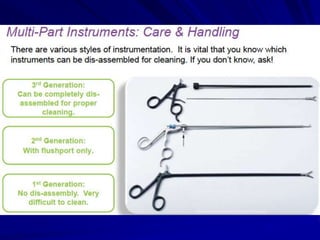
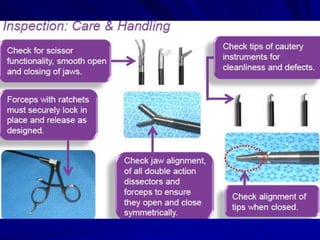
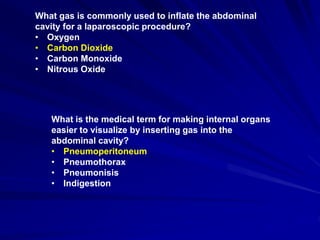
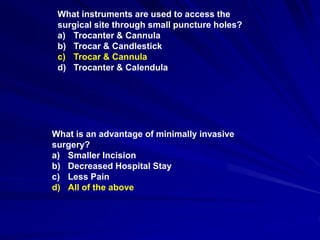
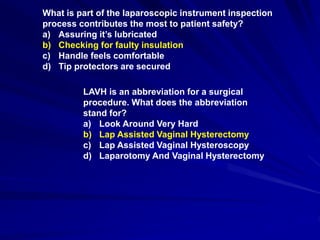
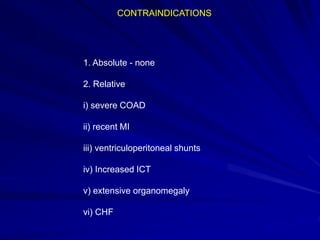
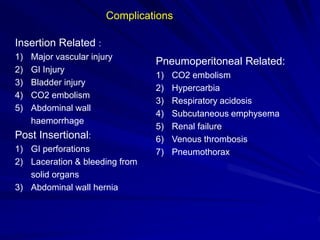
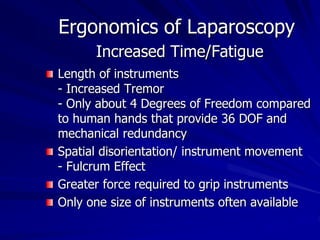
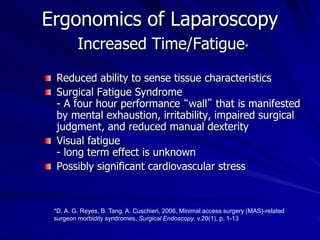
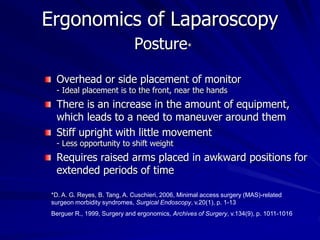
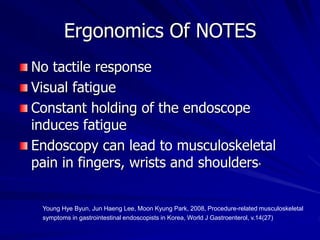
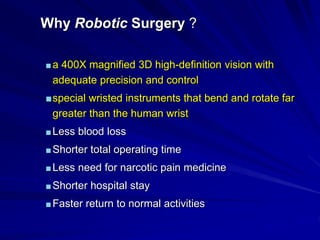
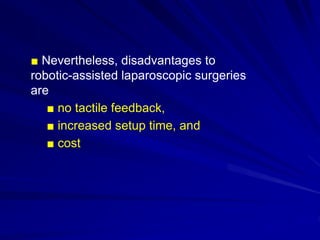
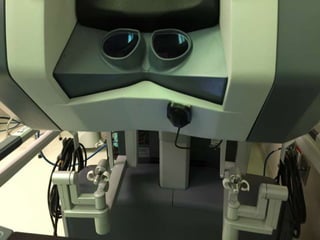
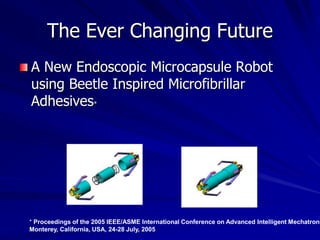
This document discusses laparoscopic surgery, a minimally invasive procedure that allows access to the peritoneal cavity for operations using small incisions and a laparoscope. It covers the history, instruments, advantages, and complications of laparoscopic procedures, emphasizing the importance of proper instrument handling and decontamination to ensure patient safety. The document also outlines the ergonomics and challenges faced by surgeons during laparoscopic surgeries, including the benefits and drawbacks of robotic-assisted laparoscopic techniques.