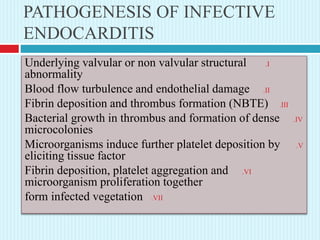
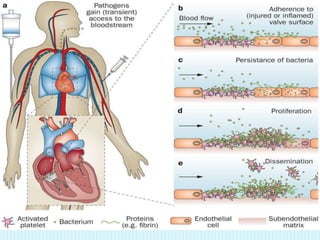
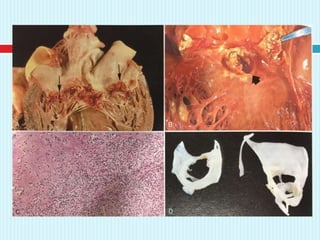
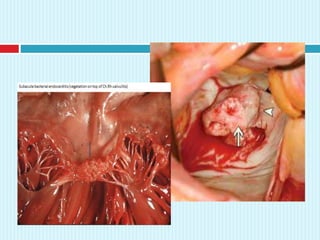
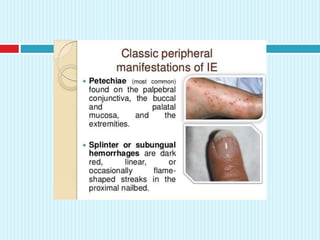
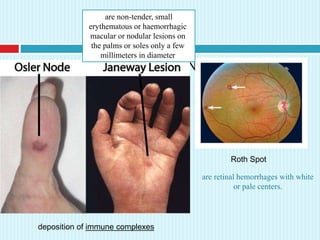
This document discusses infective endocarditis, including its risk factors, classification, typical causative organisms, pathogenesis, clinical manifestations, diagnosis, and treatment. Some key points:
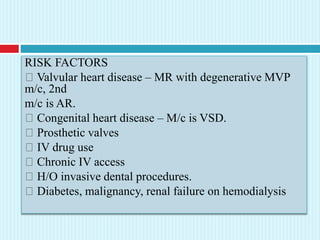
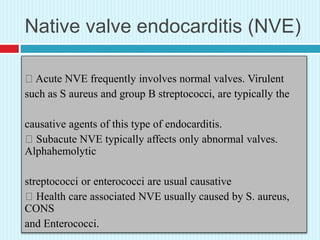
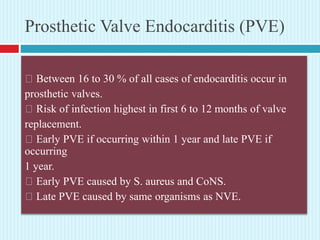
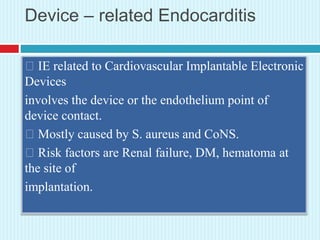
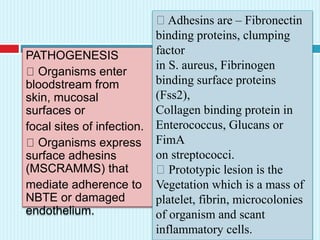
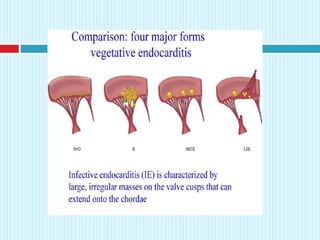
- Infective endocarditis is an infection of the endocardial surface of the heart that can involve heart valves or other structures. Risk factors include valvular heart disease, congenital heart disease, IV drug use, and prosthetic valves.
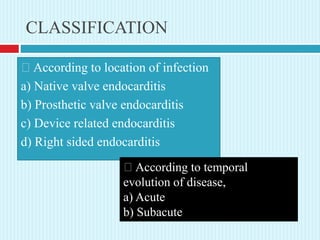
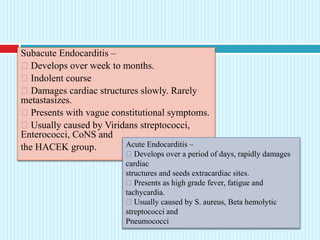
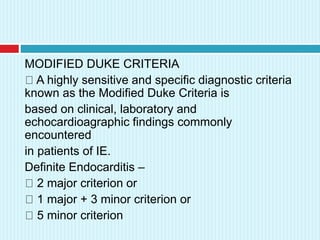
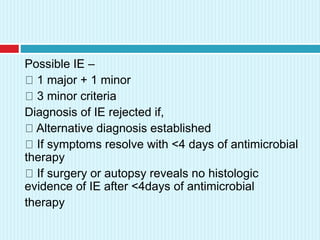
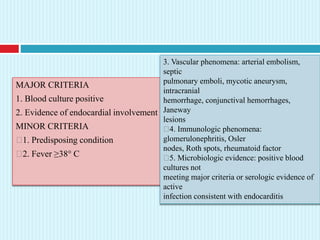
- It is classified based on location (native valve, prosthetic valve, etc.), temporal evolution (acute or subacute), and according to guidelines known as the Modified Duke Criteria for diagnosis.
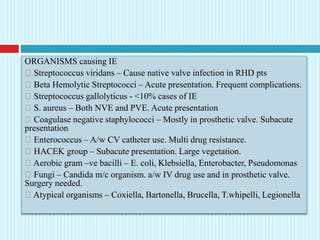
- Common causative organisms include streptococci, staphylococ