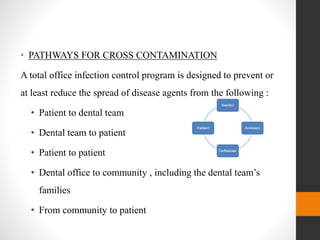
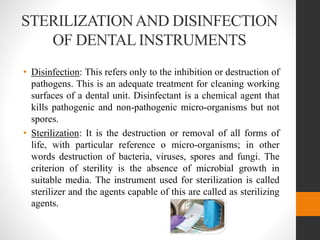
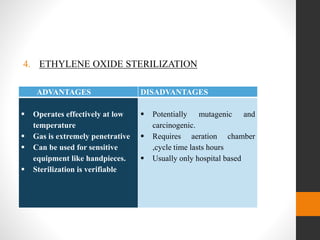
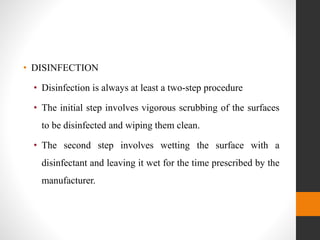
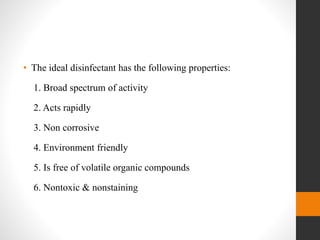
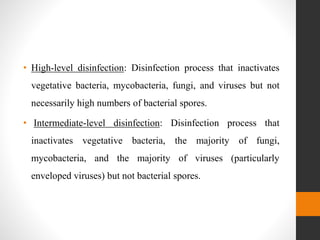
This document provides an overview of infection control in dentistry. It discusses the development of infectious diseases, oral microbiology, and rationales for infection control regulations. The key points are: infection occurs when a pathogen enters the body and grows, causing damage; dental practices implement preventive measures to break the chain of infection; and the goal of infection control is to reduce pathogen exposure and transmission between patients and staff through measures like sterilization, barriers, and hygiene.
![[fromMillerCH,CottoneJC:DentClinNorthAm37:1-20,1993]
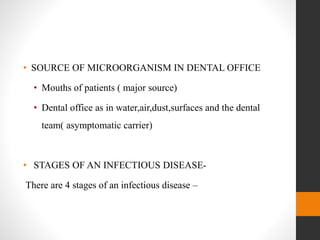
Source of microorganism
Escape of microorganism from the source
Spread of microorganism to a new person
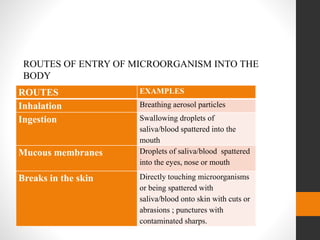
Entry of microorganism into the person
Infection ( survival and growth of microorganism)
Damage to the body](https://image.slidesharecdn.com/ayushiseminar2infectioncontrol-210726090207/85/infection-control-6-320.jpg)