The document discusses the immediate loading protocol in dental implants, highlighting the evolution of surgical techniques to enhance treatment efficiency and patient needs. It outlines indications, contraindications, and the factors affecting immediate loading, emphasizing the importance of primary stability and bone quality. Also covered are the advantages and disadvantages of immediate loading, along with the rationale for its application in implant dentistry.
![• Reduction in Time of Therapy.
• One stage surgical approach
• Patient does not need to wear removable prosthesis during
osseointegration
• Preservation of The Bone and Gingival Tissues. [facilitates soft tissue
shaping ]
• Psychological factors, function & stability also enhanced
ADVANTAGES
• Schneider RL, Higginbottom FL, Webber H, Sones AD: For your patients receiving endosseous implants for immediate loading, how are the implant-supported crowns or the prosthesis initially put into occlusal function, and what
instructions are given for their use. Int J Oral Maxillofac Imp 2002; 17:881-4.
• Bhola, M., Neely, A. L., & Kolhatkar, S Immediate Implant Placement: Clinical Decisions, Advantages, and Disadvantages. Journal of Prosthodontics, 2008 17(7), 576–581.](https://image.slidesharecdn.com/11immediateimplantloading-241012184252-66c8fcb7/85/Immediate-implant-loading-protocols-pptx-11-320.jpg)
![DISADVANTAGES
More patient co-operation is needed.
Inadequate Soft Tissue Coverage.
Parafunctional from tongue or foreign bodies [pen biting ] may cause
trauma and crestal bone loss
Peri-implant bone reaction is highest after surgical trauma due to
immediate loading.
Difficulty Obtaining Primary Stability.
Too soft bone ,small implant diameters or implant design with less
surface area ,may cause too great crestal bone stress contours and
cause bone loss or implant failure
• Schneider RL, Higginbottom FL, Webber H, Sones AD: For your patients receiving endosseous implants for immediate loading, how are the implant-supported crowns or the prosthesis initially put into occlusal function, and what
instructions are given for their use. Int J Oral Maxillofac Imp 2002; 17:881-4.
• Bhola, M., Neely, A. L., & Kolhatkar, S Immediate Implant Placement: Clinical Decisions, Advantages, and Disadvantages. Journal of Prosthodontics, 2008 17(7), 576–581.](https://image.slidesharecdn.com/11immediateimplantloading-241012184252-66c8fcb7/85/Immediate-implant-loading-protocols-pptx-12-320.jpg)
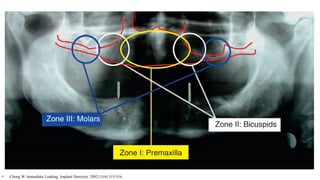
![MAXILLA
• According to Bedrossian et al. [2008], the maxilla can be divided into three zones:
zone 1, the premaxilla; zone 2, the premolar area; and zone 3, the molar area
• CBCT can be used to determine the amount of bone in these zones as well as in
the zygomatic arch, in both horizontal and vertical dimensions. Moreover, any
pathology in these areas, as well as in the maxillary sinuses, needs to be verified
preoperatively.
• Misch C. Contemporary Implant Dentistry. Implant Dentistry. 1999;8(1):90.
• Chong W. Immediate Loading. Implant Dentistry. 2002;11(4):315-316](https://image.slidesharecdn.com/11immediateimplantloading-241012184252-66c8fcb7/85/Immediate-implant-loading-protocols-pptx-38-320.jpg)

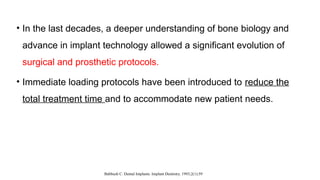
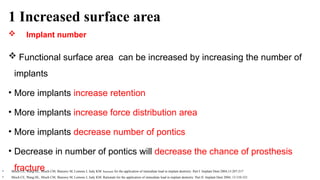
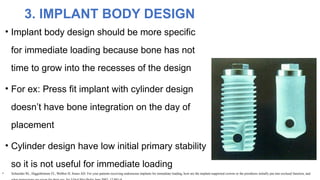
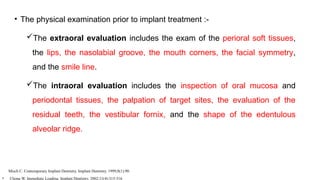
![Implant number
increase
• increase the surface area
• increase retention
• increase force distribution area
• Decrease in number of pontics will decrease the chance of
prosthesis fracture
Implant size can
be increased
either by length
or by width
• Wider implants provides greater surface area and reduce
crestal bone loss
• Long implants also permit to engage in the opposite cortical
plate, which further increase primary stability
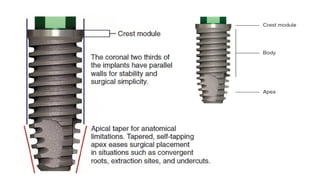
Implant body
design
• greater the number of depth and threads, the greater the
functional surface area
Implant surface
condition
• Hydroxyapatite –coated implants in poor density types
• Rough versus smooth or machine surface condition implants
in good bone density situations [D2,D3]
CONCLUSION](https://image.slidesharecdn.com/11immediateimplantloading-241012184252-66c8fcb7/85/Immediate-implant-loading-protocols-pptx-53-320.jpg)