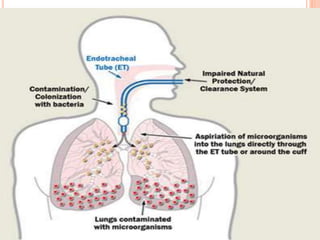
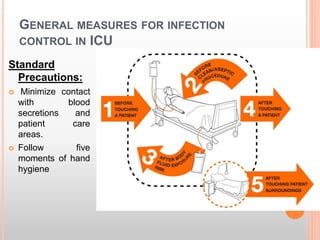
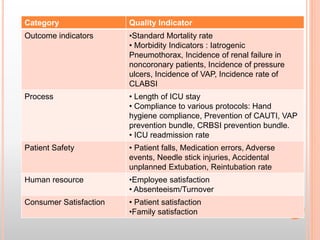
The document details infection control measures in ICU settings, emphasizing the high risk of hospital-acquired infections that can lead to significant morbidity and mortality. Key types of infections include ventilator-associated pneumonia (VAP), catheter-associated infections, and bloodstream infections, with various prevention protocols outlined for each category. It also highlights the importance of adhering to hygiene standards, proper waste disposal, and maintaining a clean environment to mitigate infection risks within critical care units.