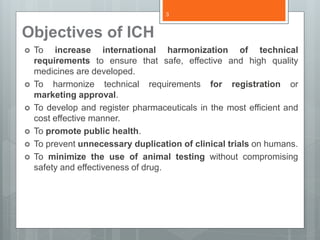
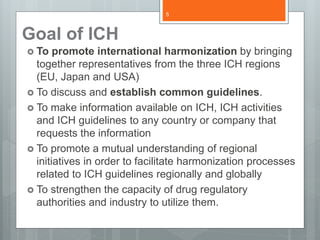
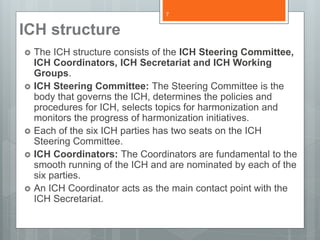
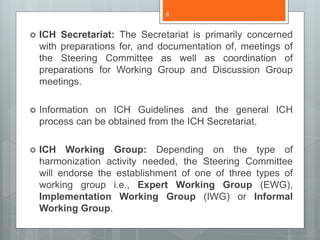
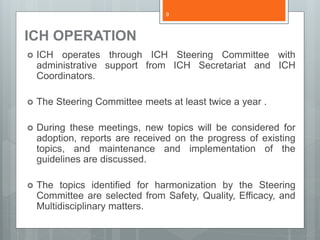
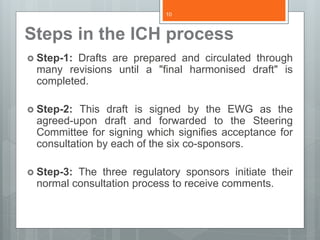
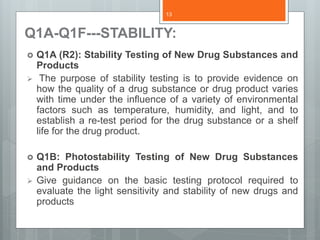
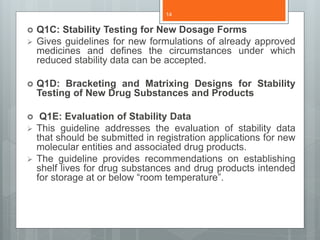
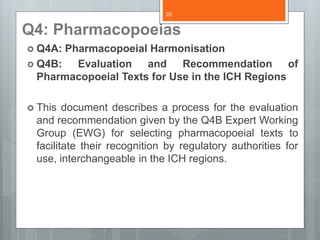
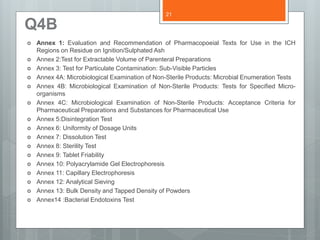
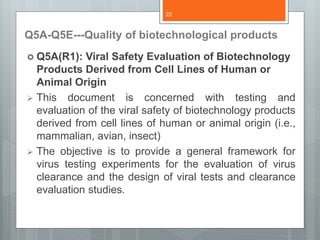
The document provides information on the International Conference on Harmonization (ICH). ICH is an initiative to discuss and establish common guidelines for pharmaceutical product registration requirements between regulators in the EU, Japan, and the US. The objectives of ICH include increasing international harmonization of technical requirements to ensure safe, effective, and high-quality medicines and minimizing duplication of clinical trials. ICH guidelines cover topics like quality, safety, efficacy, and multidisciplinary issues.